Newsroom
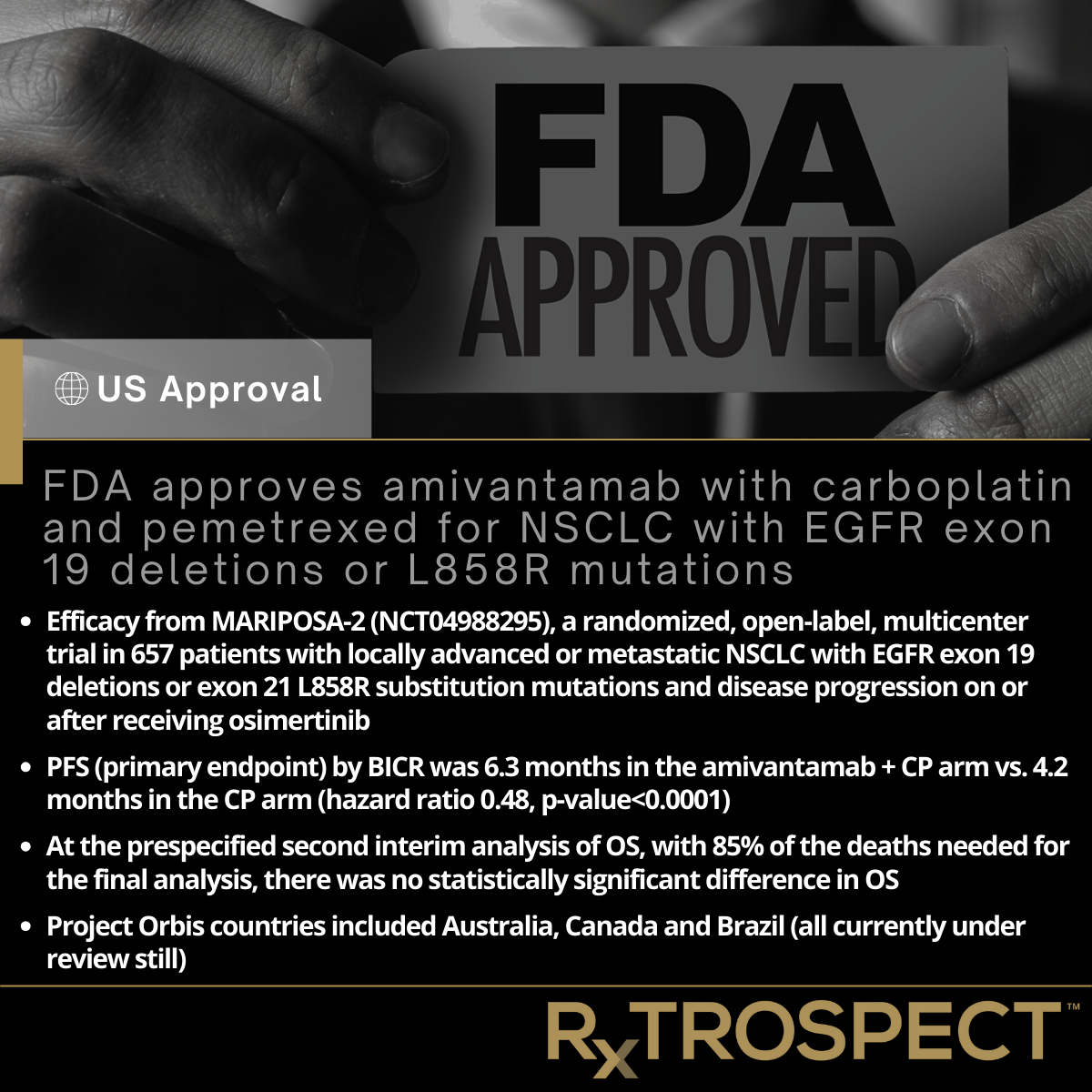
FDA approves amivantamab with carboplatin and pemetrexed for NSCLC with EGFR exon 19 deletions or L858R mutations
FDA approves amivantamab with carboplatin and pemetrexed for NSCLC with EGFR exon 19 deletions or L858R mutations
Efficacy from MARIPOSA-2 (NCT04988295), a randomized, open-label, multicenter trial in 657 patients with locally advanced or metastatic NSCLC with EGFR exon 19 deletions or exon 21 L858R substitution mutations and disease progression on or after receiving osimertinib.
PFS (primary endpoint) by BICR was 6.3 months in the amivantamab + CP arm vs. 4.2 months in the CP arm (hazard ratio 0.48, p-value<0.0001).
At the prespecified second interim analysis of OS, with 85% of the deaths needed for the final analysis, there was no statistically significant difference in OS.
Project Orbis countries included Australia, Canada and Brazil (all currently under review still).
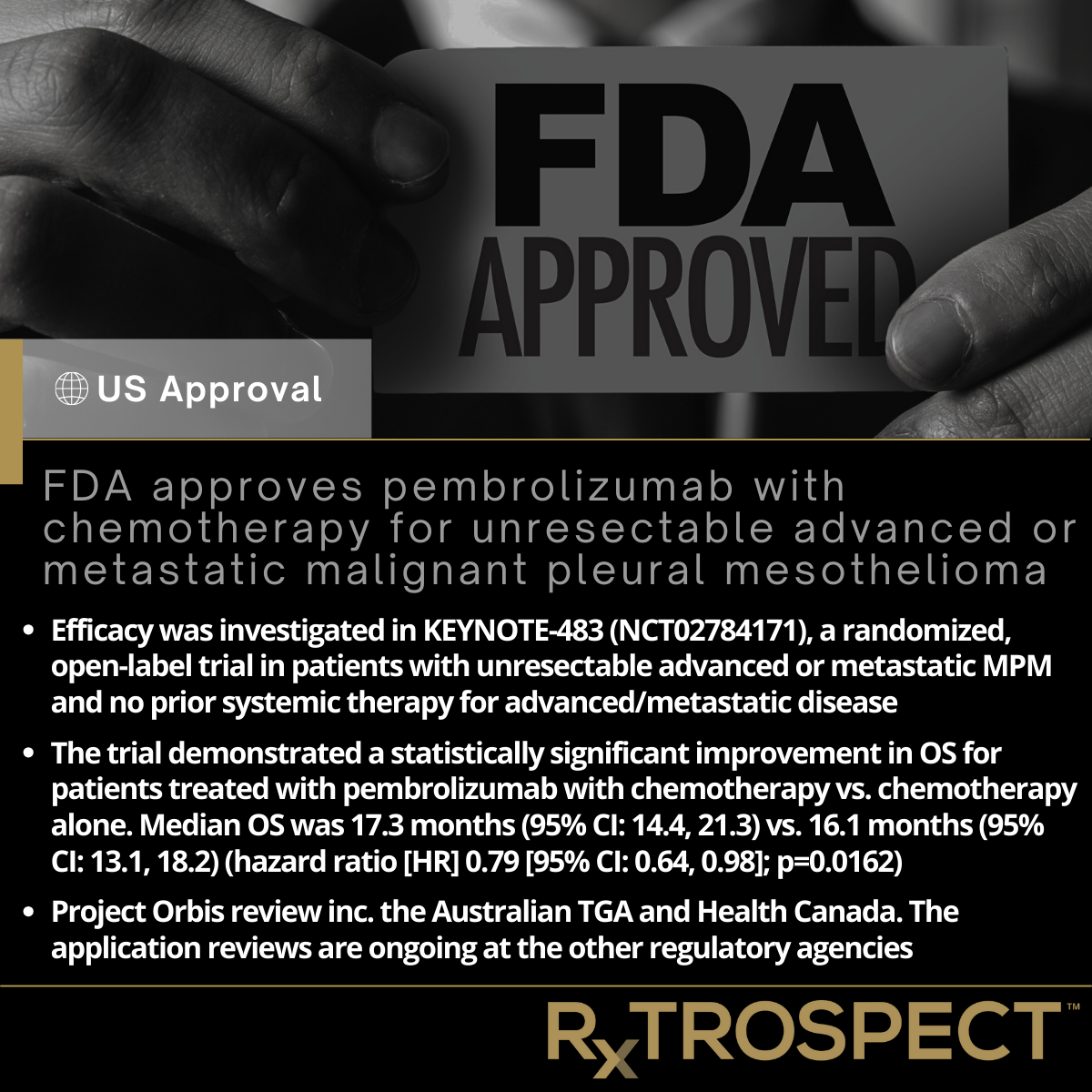
FDA approves pembrolizumab with chemotherapy for unresectable advanced or metastatic malignant pleural mesothelioma
FDA approves pembrolizumab with chemotherapy for unresectable advanced or metastatic malignant pleural mesothelioma
Efficacy was investigated in KEYNOTE-483 (NCT02784171), a randomized, open-label trial in patients with unresectable advanced or metastatic MPM and no prior systemic therapy for advanced/metastatic disease
The trial demonstrated a statistically significant improvement in OS for patients treated with pembrolizumab with chemotherapy vs. chemotherapy alone. Median OS was 17.3 months (95% CI: 14.4, 21.3) vs. 16.1 months (95% CI: 13.1, 18.2) (hazard ratio [HR] 0.79 [95% CI: 0.64, 0.98]; p=0.0162).
Project Orbis review inc. the Australian TGA and Health Canada. The application reviews are ongoing at the other regulatory agencies.
FDA approves Kisqali with an aromatase inhibitor & Kisqali Femara Co-Pack for early high-risk breast cancer
FDA approves Kisqali with an aromatase inhibitor & Kisqali Femara Co-Pack for early high-risk breast cancer
FDA approved Kisqali (ribociclib, Novartis) with an aromatase inhibitor for the adjuvant treatment of adults with HR-positive, HER2-negative stage II and III early breast cancer at high risk of recurrence.
Efficacy of ribociclib with a non-steroidal aromatase inhibitor was evaluated in NATALEE (NCT03701334), a randomized, open-label, multicenter trial in 5101 adults with HR-positive, HER2-negative early breast cancer.
Efficacy results at the final iDFS analysis showed that iDFS at 36 months was 90.7% (95% CI: 89.3, 91.8) in the ribociclib + NSAI arm and 87.6% (95% CI: 86.1, 88.9) in the NSAI arm, HR 0.749 (95% CI: 0.628, 0.892). At the time of the iDFS final analysis, OS was immature.
Additionally, FDA also approved the ribociclib and letrozole co-pack for the same indication.
European Commission Approves Astellas’ PADCEV in Combination with KEYTRUDA for First-Line Treatment of Advanced Urothelial Cancer
European Commission Approves Astellas’ PADCEV in Combination with KEYTRUDA for First-Line Treatment of Advanced Urothelial Cancer
First regimen approved in advanced UC to demonstrate superiority to platinum-containing chemotherapy, the standard of care for nearly 40 years
European MA based on positive overall survival and progression-free survival results from the global Phase 3 EV-302 trial
median OS of 31.5 months compared to 16.1 months with platinum-containing chemotherapy, representing a 53% reduction in risk of death (Hazard Ratio [HR]=0.47; 95% Confidence Interval [CI]: 0.38-0.58; P<0.00001).
PFS of 12.5 months for the combination compared to 6.3 months with chemotherapy represents a 55% reduction in the risk of cancer progression or death (HR=0.45; 95% CI: (0.38-0.54); P<0.00001)
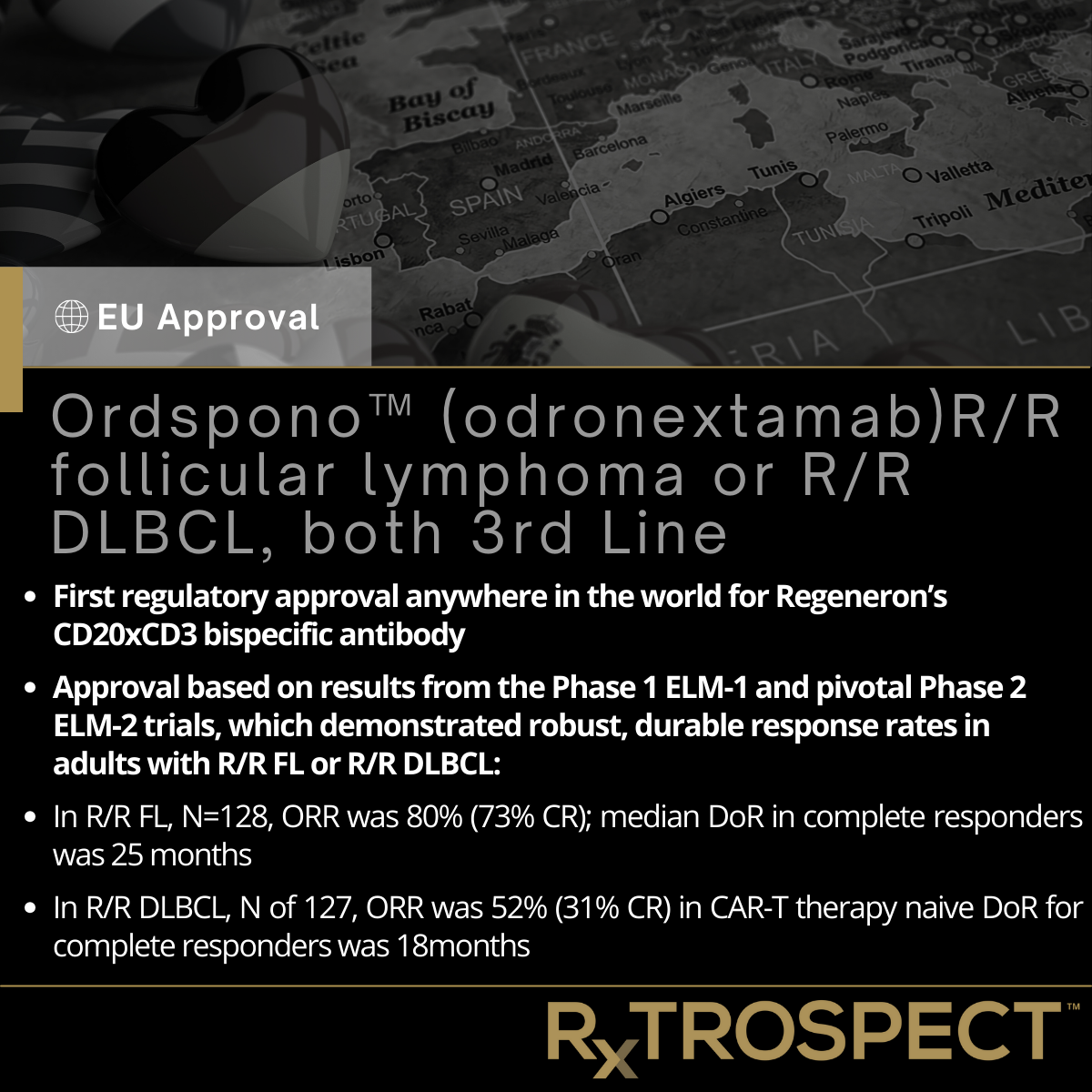
Ordspono™ (odronextamab)R/R follicular lymphoma or R/R DLBCL, both 3rd Line
Ordspono™ (odronextamab)R/R follicular lymphoma or R/R DLBCL, both 3rd Line
First regulatory approval anywhere in the world for Regeneron’s CD20xCD3 bispecific antibody
Approval based on results from the Phase 1 ELM-1 and pivotal Phase 2 ELM-2 trials, which demonstrated robust, durable response rates in adults with R/R FL or R/R DLBCL:
In R/R FL, N=128, ORR was 80% (73% CR); median DoR in complete responders was 25 months
In R/R DLBCL, N of 127, ORR was 52% (31% CR) in CAR-T therapy naive DoR for complete responders was 18months
FDA Approves RYBREVANT (amivantamab) plus LAZCLUZE (lazertinib) in first-line chemotherapy-free treatment for patients with EGFR-mutated NSCLC
FDA Approves RYBREVANT (amivantamab) plus LAZCLUZE (lazertinib) in first-line chemotherapy-free treatment for patients with EGFR-mutated NSCLC
Combination demonstrated a statistically significant improvement in PFS vs. osimertinib with a hazard ratio of 0.70; p-value=0.0002). The median PFS was 23.7 months vs. 16.6 months.
No detriment was observed in OS.
Project Orbis review inc. Australia, Brazil, Canada, Switzerland and the UK.
Longer-term follow-up data from the Phase 3 MARIPOSA will be presented IASLC 2024 WCLC next month.
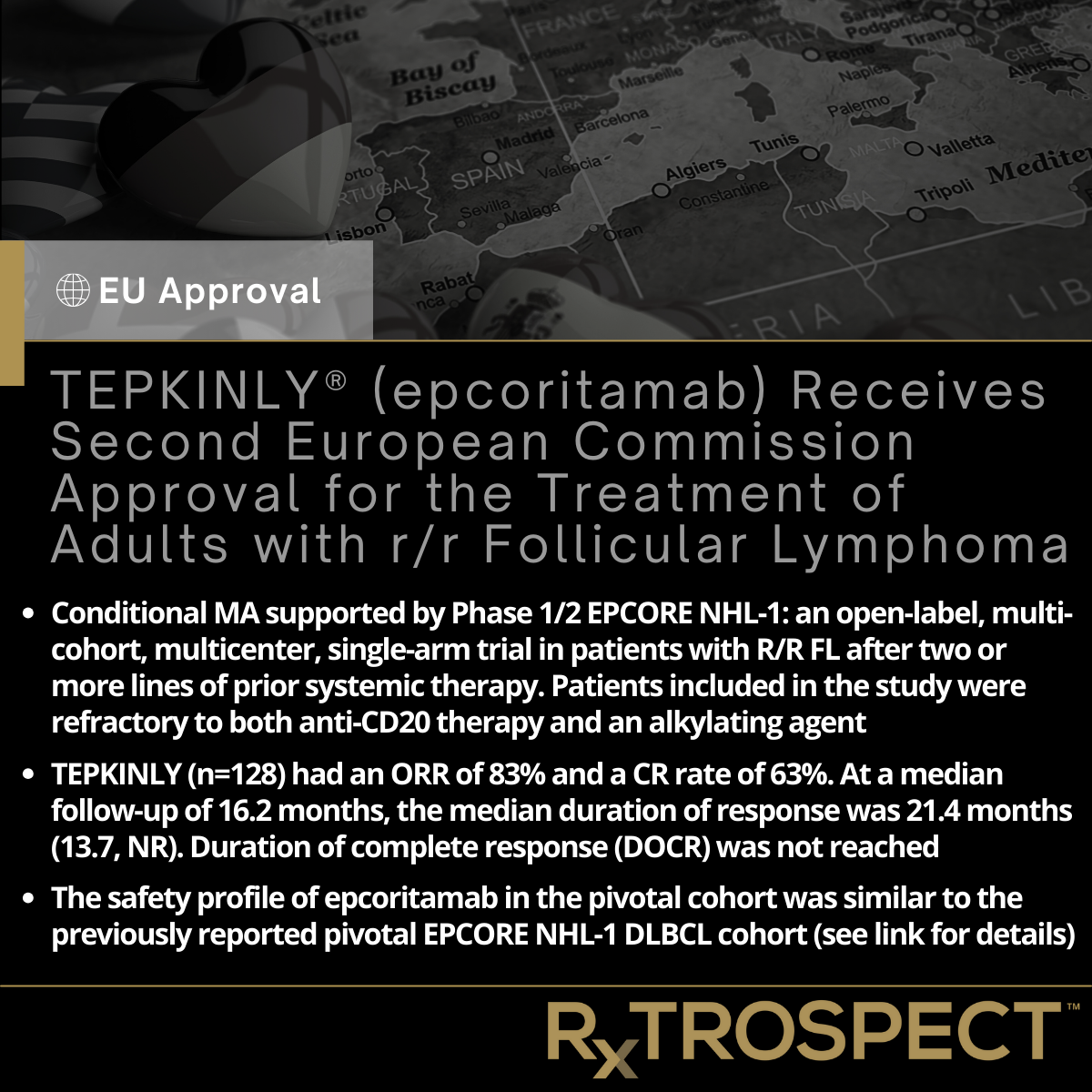
TEPKINLY® (epcoritamab) Receives Second European Commission Approval for the Treatment of Adults with r/r Follicular Lymphoma
TEPKINLY® (epcoritamab) Receives Second European Commission Approval for the Treatment of Adults with r/r Follicular Lymphoma
Conditional MA supported by Phase 1/2 EPCORE NHL-1: an open-label, multi-cohort, multicenter, single-arm trial in patients with R/R FL after two or more lines of prior systemic therapy. Patients included in the study were refractory to both anti-CD20 therapy and an alkylating agent.
TEPKINLY (n=128) had an ORR of 83% and a CR rate of 63%. At a median follow-up of 16.2 months, the median duration of response was 21.4 months (13.7, NR). Duration of complete response (DOCR) was not reached.
The safety profile of epcoritamab in the pivotal cohort was similar to the previously reported pivotal EPCORE NHL-1 DLBCL cohort (see link for details).
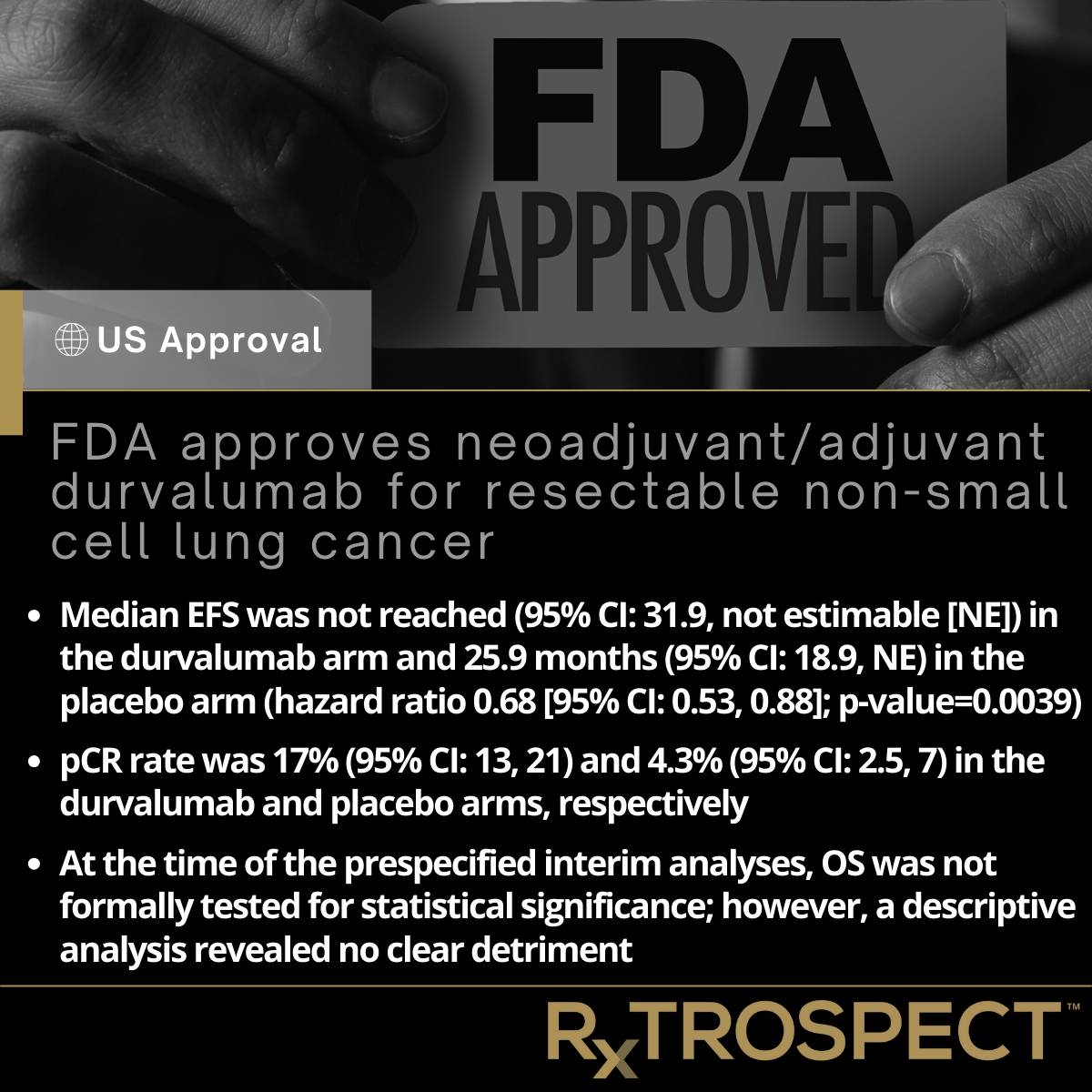
FDA approves neoadjuvant/adjuvant durvalumab for resectable non-small cell lung cancer
FDA approves neoadjuvant/adjuvant durvalumab for resectable non-small cell lung cancer
Median EFS was not reached (95% CI: 31.9, not estimable [NE]) in the durvalumab arm and 25.9 months (95% CI: 18.9, NE) in the placebo arm (hazard ratio 0.68 [95% CI: 0.53, 0.88]; p-value=0.0039).
pCR rate was 17% (95% CI: 13, 21) and 4.3% (95% CI: 2.5, 7) in the durvalumab and placebo arms, respectively.
At the time of the prespecified interim analyses, OS was not formally tested for statistical significance; however, a descriptive analysis revealed no clear detriment.