Newsroom
European Commission Approve First China Domestic anti-PD-L1 mAb sugemalimab as First-Line Treatment for Non-Small Cell Lung Cancer
European Commission Approve First China Domestic anti-PD-L1 mAb sugemalimab as First-Line Treatment for Non-Small Cell Lung Cancer
Sugemalimab becomes the world’s first anti-PD-L1 mAb approved in Europe for first-line treatment of both squamous and non-squamous non-small cell lung cancer (NSCLC), also marking the first successful international approval of a China domestic anti-PD-L1 mAb.
EU approval is based on the results of GEMSTONE-302 Phase 3 trial, which demonstrated that sugemalimab in combination with chemotherapy significantly prolonged PFS in treatment-naive patients with metastatic NSCLC.
All participants were Asian and had Stage IV NSCLC; the median age was 63.0 years; 80.0% were males; 73.3% were former or current smokers.
CStone is actively preparing to submit additional applications in Europe for new indications, including Stage III NSCLC, first-line Gastric Cancer, first-line Esophageal Cancer, and relapsed/refractory extranodal natural killer/T-cell lymphoma (r/r ENKTL).
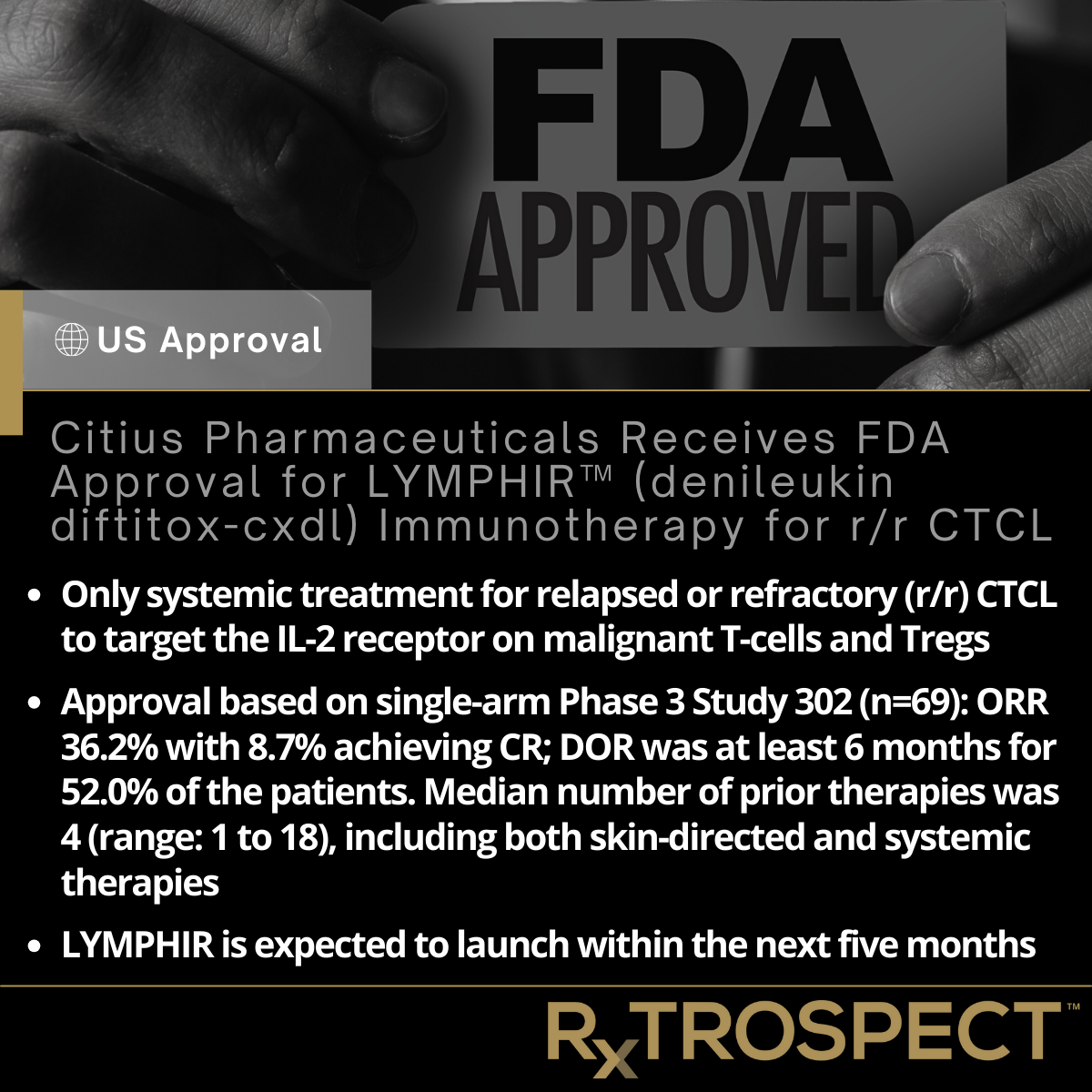
Citius Pharmaceuticals Receives FDA Approval for LYMPHIR™ (denileukin diftitox-cxdl) Immunotherapy for r/r CTCL
Citius Pharmaceuticals Receives FDA Approval for LYMPHIR™ (denileukin diftitox-cxdl) Immunotherapy for r/r CTCL
Only systemic treatment for relapsed or refractory (r/r) CTCL to target the IL-2 receptor on malignant T-cells and Tregs
Approval based on single-arm Phase 3 Study 302 (n=69): ORR 36.2% with 8.7% achieving CR; DOR was at least 6 months for 52.0% of the patients. Median number of prior therapies was 4 (range: 1 to 18), including both skin-directed and systemic therapies
LYMPHIR is expected to launch within the next five months
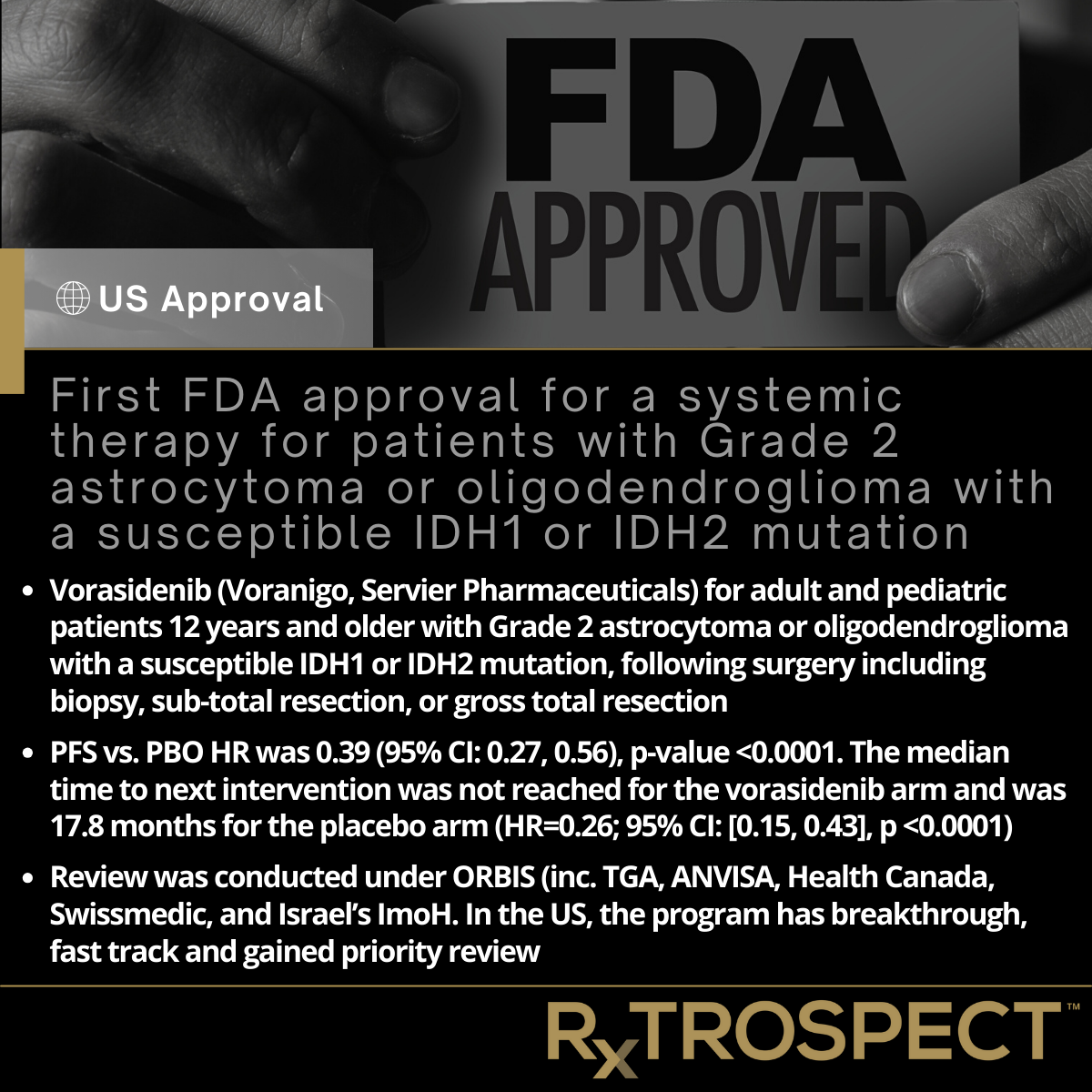
First FDA approval for a systemic therapy for patients with Grade 2 astrocytoma or oligodendroglioma with a susceptible IDH1 or IDH2 mutation
First FDA approval for a systemic therapy for patients with Grade 2 astrocytoma or oligodendroglioma with a susceptible IDH1 or IDH2 mutation
Vorasidenib (Voranigo, Servier Pharmaceuticals) for adult and pediatric patients 12 years and older with Grade 2 astrocytoma or oligodendroglioma with a susceptible IDH1 or IDH2 mutation, following surgery including biopsy, sub-total resection, or gross total resection.
PFS vs. PBO HR was 0.39 (95% CI: 0.27, 0.56), p-value <0.0001. The median time to next intervention was not reached for the vorasidenib arm and was 17.8 months for the placebo arm (HR=0.26; 95% CI: [0.15, 0.43], p <0.0001).
Review was conducted under ORBIS (inc. TGA, ANVISA, Health Canada, Swissmedic, and Israel’s ImoH. In the US, the program has breakthrough, fast track and gained priority review.
FDA Approves First Gene Therapy to Treat Adults with Metastatic Synovial Sarcoma
FDA Approves First Gene Therapy to Treat Adults with Metastatic Synovial Sarcoma
Accelerated approval based on multicenter, open-label trial including 44 patients with inoperable and metastatic synovial sarcoma who had received prior systemic therapy and whose tumor expressed the MAGE-A4 tumor antigen.
ORR was 43.2% and the median DOR was six months.
The FDA granted Adaptimmune’s Tecelra Orphan Drug, Regenerative Medicine Advanced Therapy and Priority Review designations for this indication. This application was reviewed using a coordinated, cross-agency approach, including CBER, the FDA’s Oncology CoE and the CDRH
Tecelra is also the first FDA-approved T cell receptor (TCR) gene therapy. The product is an autologous T cell immunotherapy composed of a patient’s own T cells. T cells in Tecelra are modified to express a TCR that targets MAGE-A4, an antigen (substance that normally triggers your immune system) expressed by cancer cells in synovial sarcoma. The product is administered as a single intravenous dose.
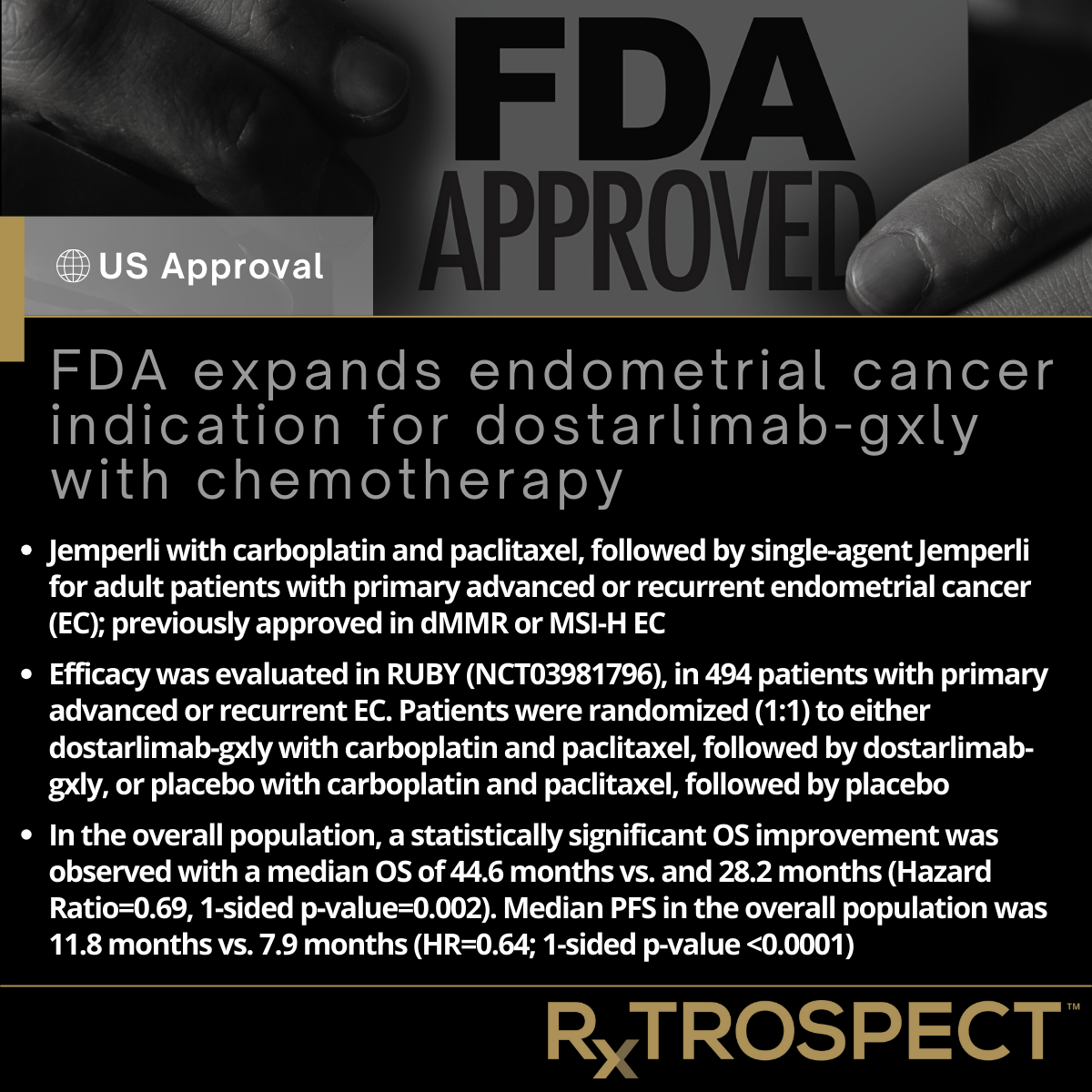
FDA expands endometrial cancer indication for dostarlimab-gxly with chemotherapy
FDA expands endometrial cancer indication for dostarlimab-gxly with chemotherapy
Jemperli with carboplatin and paclitaxel, followed by single-agent Jemperli for adult patients with primary advanced or recurrent endometrial cancer (EC); previously approved in dMMR or MSI-H EC.
Efficacy was evaluated in RUBY (NCT03981796), in 494 patients with primary advanced or recurrent EC. Patients were randomized (1:1) to either dostarlimab-gxly with carboplatin and paclitaxel, followed by dostarlimab-gxly, or placebo with carboplatin and paclitaxel, followed by placebo.
In the overall population, a statistically significant OS improvement was observed with a median OS of 44.6 months vs. and 28.2 months (Hazard Ratio=0.69, 1-sided p-value=0.002). Median PFS in the overall population was 11.8 months vs. 7.9 months (HR=0.64; 1-sided p-value <0.0001).
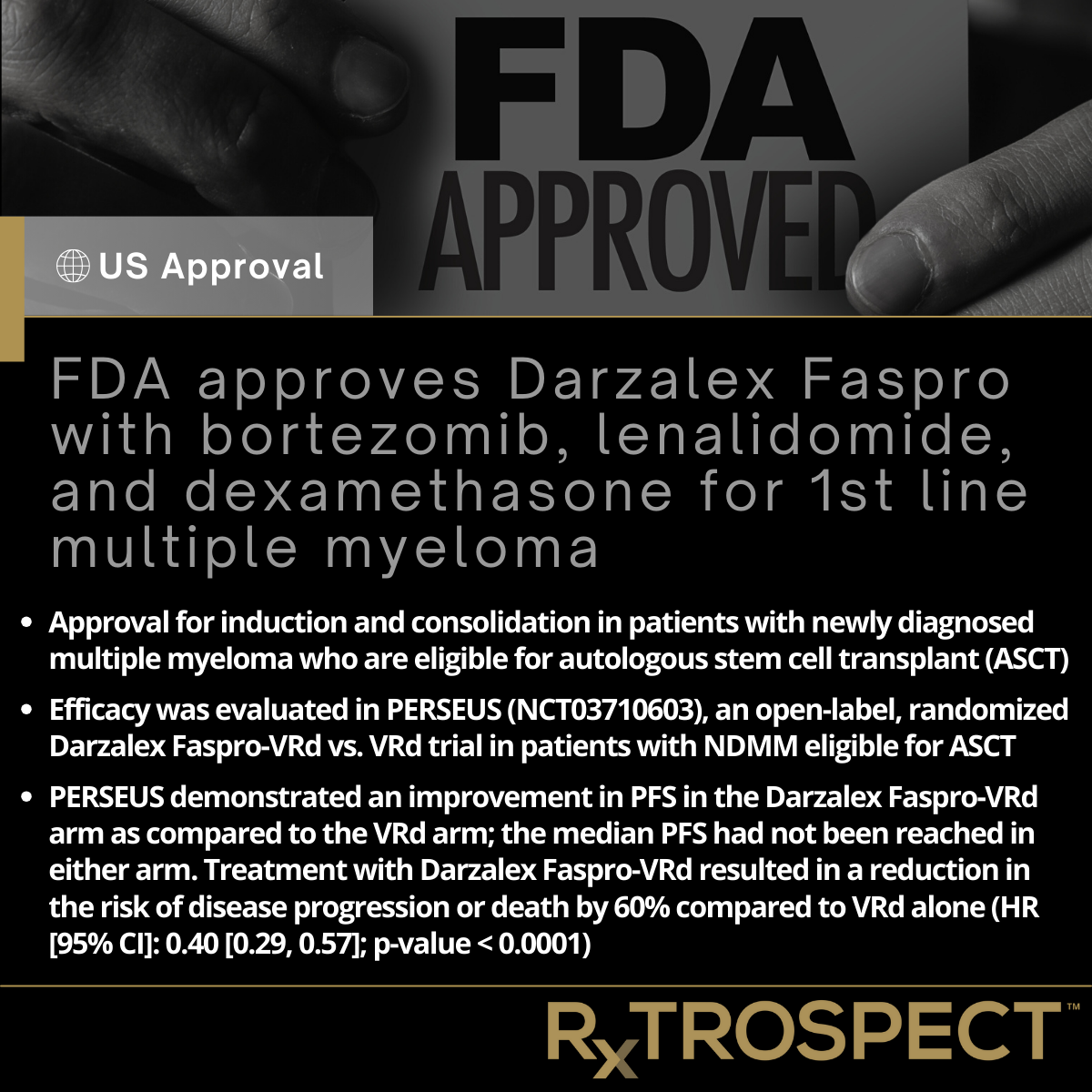
FDA approves Darzalex Faspro with bortezomib, lenalidomide, and dexamethasone for 1st line multiple myeloma
FDA approves Darzalex Faspro with bortezomib, lenalidomide, and dexamethasone for 1st line multiple myeloma
Approval for induction and consolidation in patients with newly diagnosed multiple myeloma who are eligible for autologous stem cell transplant (ASCT).
Efficacy was evaluated in PERSEUS (NCT03710603), an open-label, randomized Darzalex Faspro-VRd vs. VRd trial in patients with NDMM eligible for ASCT
PERSEUS demonstrated an improvement in PFS in the Darzalex Faspro-VRd arm as compared to the VRd arm; the median PFS had not been reached in either arm. Treatment with Darzalex Faspro-VRd resulted in a reduction in the risk of disease progression or death by 60% compared to VRd alone (HR [95% CI]: 0.40 [0.29, 0.57]; p-value < 0.0001).
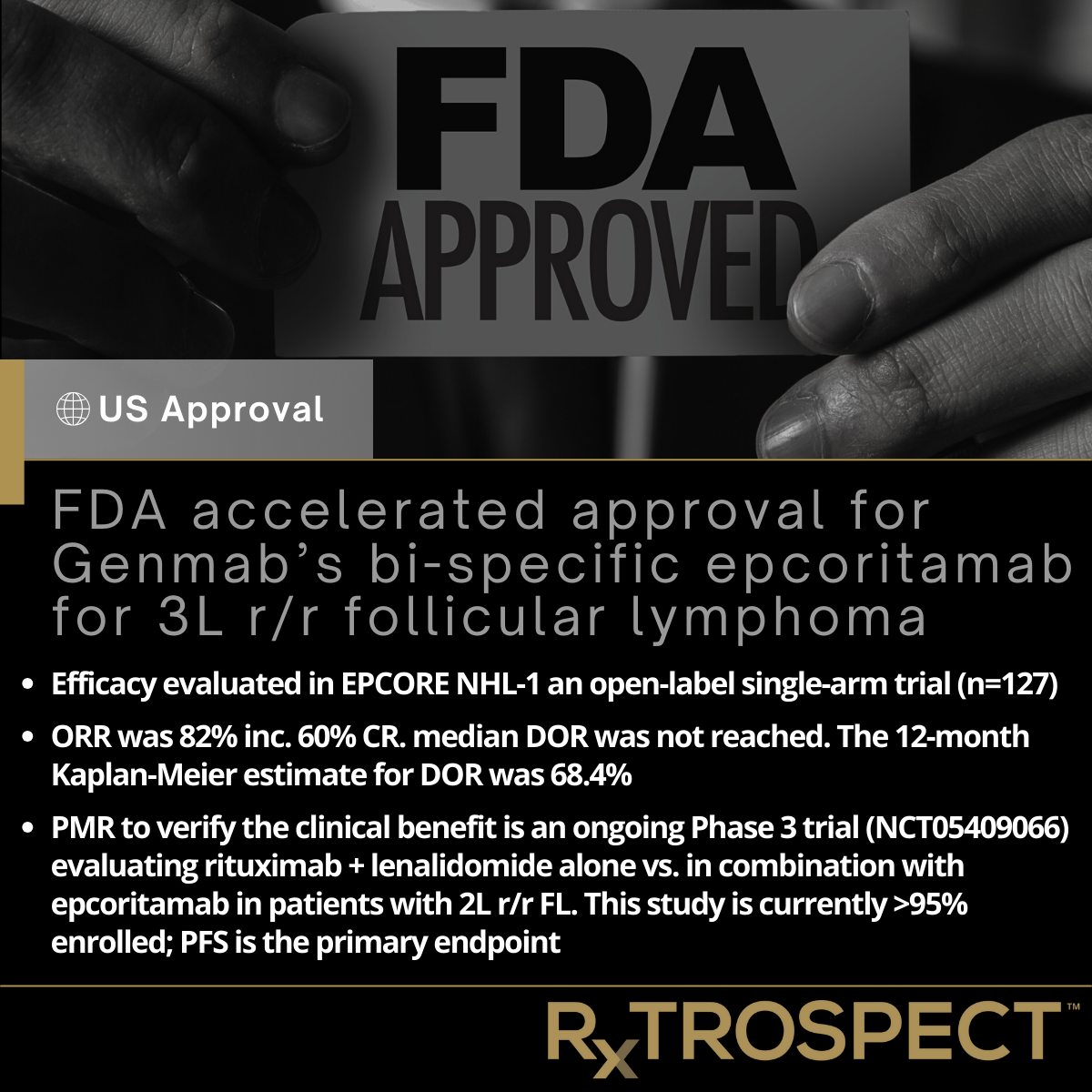
FDA accelerated approval for Genmab’s bi-specific epcoritamab for 3L r/r follicular lymphoma
FDA accelerated approval for Genmab’s bi-specific epcoritamab for 3L r/r follicular lymphoma
Efficacy evaluated in EPCORE NHL-1 an open-label single-arm trial (n=127)
ORR was 82% inc. 60% CR. median DOR was not reached. The 12-month Kaplan-Meier estimate for DOR was 68.4%
PMR to verify the clinical benefit is an ongoing Phase 3 trial (NCT05409066) evaluating rituximab + lenalidomide alone vs. in combination with epcoritamab in patients with 2L r/r FL. This study is currently >95% enrolled; PFS is the primary endpoint
European Approval for Takeda's FRUZAQLA in Previously Treated Metastatic Colorectal Cancer
European Approval for Takeda's FRUZAQLA in Previously Treated Metastatic Colorectal Cancer
Approval is based on Phase 3 FRESCO-2 trial of FRUZAQLA (fruquintinib) + BSC vs. PBO in patients with previously treated mCRC
Median OS was 7·4 months (95% CI 6·7–8·2) in the fruquintinib group versus 4·8 months (4·0–5·8) in PBO (HR 0·66, 95% CI 0·55–0·80; p<0·0001)
Approval follows Nov 2023 FDA approval for adults with mCRC who have been previously treated with oxaliplatin- and irinotecan-based regimens