Newsroom
FDA Grant Accelerated Approval to CAR-T Breyanzi in 3L r/r Follicular Lymphoma
FDA Grant Accelerated Approval to CAR-T Breyanzi in 3L r/r Follicular Lymphoma
AA based on ORR from Phase 2, single-arm TRANSCEND-FL (NCT04245839) in adults with relapsed or refractory FL after two or more lines of systemic therapy.
Remarkably, ORR was 95.7% (95% CI: 89.5, 98.8). After a median follow up of 16.8 months, median DOR was not reached (95% CI: 18.04, NR).
Most common nonlaboratory adverse reactions (≥20%) were cytokine release syndrome, headache, musculoskeletal pain, fatigue, constipation, and fever.
SEAGEN's Tivdak confirms benefit in recurrent or metastatic cervical cancer with disease progression on or after chemotherapy; AA PMR fulfilled
SEAGEN's Tivdak confirms benefit in recurrent or metastatic cervical cancer with disease progression on or after chemotherapy; AA PMR fulfilled
Efficacy was evaluated in innovaTV 301 (NCT04697628), an open-label, active-controlled, multicenter, randomized trial that enrolled 502 patients with recurrent or metastatic cervical cancer who had received one or two prior systemic regimens, including chemotherapy with or without bevacizumab and/or an anti-PD-(L)-1 agent
Median OS was 11.5 months (95% CI: 9.8, 14.9) vs. 9.5 months (95% CI: 7.9, 10.7) in the chemotherapy arm (HR 0.70 [95% CI: 0.54, 0.89] p-value 0.0038)
Trial’s results fulfill the post-marketing requirement of the FDA's 2021 accelerated approval for this indication
Another First as FDA grant accelerated approval to tovorafenib for patients with r/r BRAF-altered pediatric low-grade glioma
Another First as FDA grant accelerated approval to tovorafenib for patients with r/r BRAF-altered pediatric low-grade glioma
First FDA approval of a systemic therapy for the treatment of patients with pediatric LGG with BRAF rearrangements, including fusions
Efficacy was evaluated in 76 patients enrolled in FIREFLY-1 (NCT04775485), a multicenter, open-label, single-arm trial
ORR was 51% (95% CI: 40, 63) and median DoR was 13.8 months (95% CI: 11.3, not estimable)
First FDA approval of a radiopharmaceutical for pediatric patients 12+ with SSTR-positive GEP-NETs
First FDA approval of a radiopharmaceutical for pediatric patients 12+ with SSTR-positive GEP-NETs
Lutathera (lutetium Lu 177 dotatate) 2018 adult indication expanded to pediatrics 12 years+ with somatostatin receptor (SSTR)-positive gastroenteropancreatic neuroendocrine tumors (GEP-NETs), including foregut, midgut, and hindgut neuroendocrine tumors.
Approval was based on PK, dosimetry, and safety data from NETTER-P (NCT04711135), an ongoing, open-label, single-arm study in adolescent patients with locally advanced/inoperable or metastatic SSTR-positive GEP-NETs or pheochromocytoma/paraganglioma (PPGL).
Approval was also based on the extrapolation of efficacy outcomes observed in NETTER-1 (NCT01578239), which supported the original approval in adults.
NETTER-P was conducted as part of a pediatric Written Request (WR) under the Best Pharmaceuticals for Children Act (BPCA).
FDA approves Altor BioScience's Anktiva (nogapendekin alfa inbakicept) for BCG-unresponsive non-muscle invasive bladder cancer
FDA approves Altor BioScience's Anktiva (nogapendekin alfa inbakicept) for BCG-unresponsive non-muscle invasive bladder cancer
Efficacy was evaluated in QUILT-3.032 (NCT0302285), a single-arm, multicenter trial of 77 patients with BCG-unresponsive, high-risk NMIBC with CIS with or without Ta/T1 papillary disease following transurethral resection.
CR was defined by a negative cystoscopy (with TURBT/biopsies as applicable) and urine cytology. CR rate was 62% (95% CI: 51, 73). Fifty-eight percent of patients with CR had a DOR ≥ 12 months and 40% had a DOR ≥ 24 months.
The most common adverse reactions (≥15%), including laboratory test abnormalities, were increased creatinine, dysuria, hematuria, urinary frequency, micturition urgency, urinary tract infection, increased potassium, musculoskeletal pain, chills, and pyrexia.
FDA Approves Genentech's Alecensa as First Adjuvant Treatment for People With ALK-Positive Early-Stage Lung Cancer
FDA Approves Genentech's Alecensa as First Adjuvant Treatment for People With ALK-Positive Early-Stage Lung Cancer
Phase III ALINA study showed alectinib reduced the risk of disease recurrence or death by 76% (HR=0.24, 95% CI: 0.13-0.43, p<0.0001) vs. platinum-based chemotherapy in people with completely resected IB (tumor ≥ 4 cm) to IIIA ALK-positive NSCLC.
In an exploratory analysis, an improvement of central nervous system (CNS)-DFS was observed (HR=0.22; 95% CI: 0.08-0.58).
Review utilized RTOR and Project Orbis (FDA w/Australia’s TGA, Health Canada, Israel’s MoH, Swissmedic & the UK’s MHRA). Brazil's ANVISA and Singapore’s HAS will also be participating as Type C Project Orbis Partners.
CARVYKTI Becomes First and Only BCMA-Targeted Treatment Approved by the U.S. FDA in Second-line Multiple Myeloma
CARVYKTI Becomes First and Only BCMA-Targeted Treatment Approved by the U.S. FDA in Second-line Multiple Myeloma
Phase 3 CARTITUDE-4 study demonstrated earlier use of CARVYKTI® reduced the risk of disease progression or death by 59% vs. standard therapies—pomalidomide, bortezomib and dexamethasone (PVd) or daratumumab, pomalidomide and dexamethasone (DPd) in adults with relapsed and lenalidomide-refractory multiple myeloma who received one to three prior lines of therapy.
CARVYKTI received FDA approval in 2022 for more heavily pre-treated MM; this expansion of indication (unanimously supported by ODAC 11 to 0) moving the product into second-line MM.
In Europe, in February 2024 EMA's CHMP issued a positive opinion to move the therapy to second-line MM. EU approval is expected any day now.
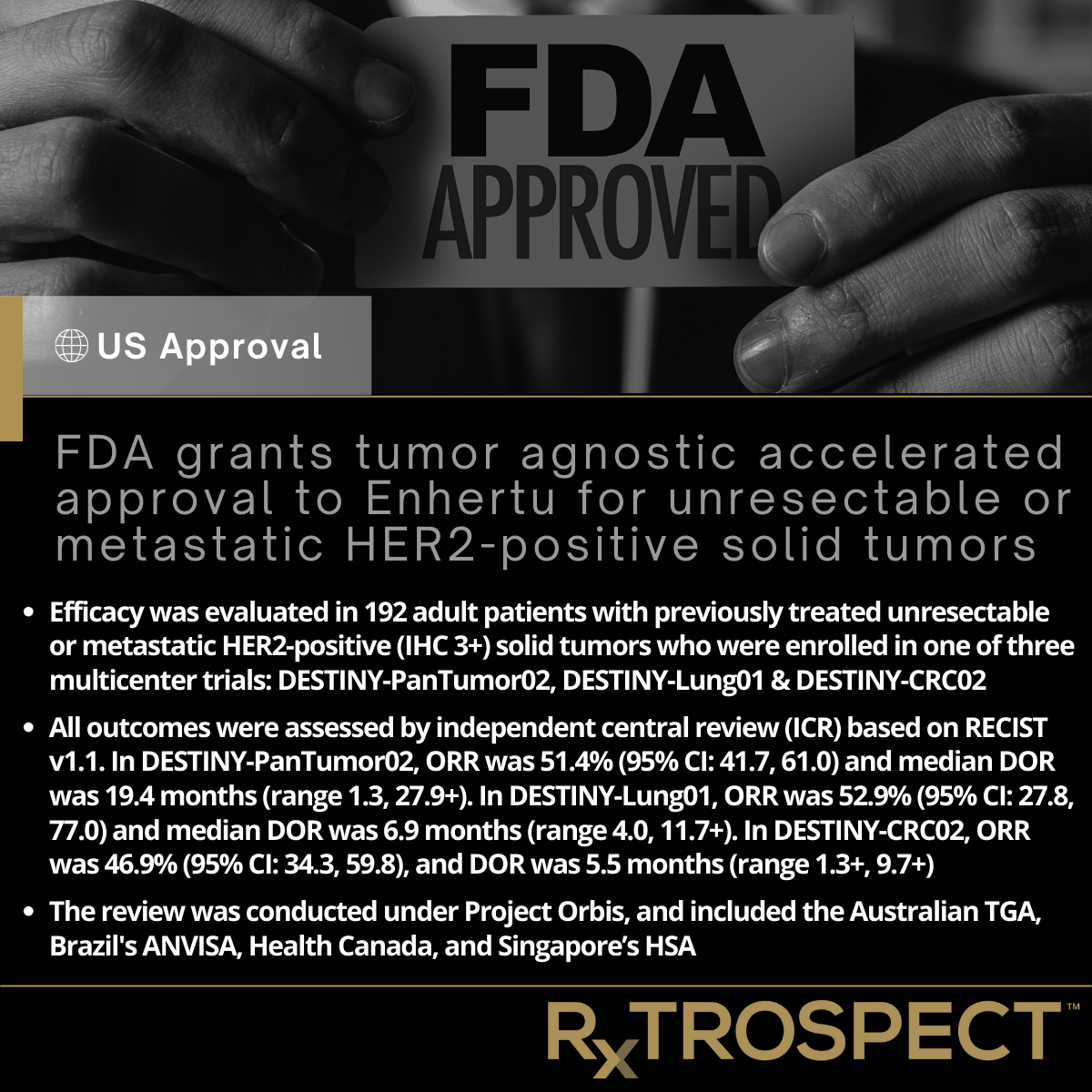
FDA grants tumor agnostic accelerated approval to Enhertu for unresectable or metastatic HER2-positive solid tumors
FDA grants tumor agnostic accelerated approval to Enhertu for unresectable or metastatic HER2-positive solid tumors
Efficacy was evaluated in 192 adult patients with previously treated unresectable or metastatic HER2-positive (IHC 3+) solid tumors who were enrolled in one of three multicenter trials: DESTINY-PanTumor02, DESTINY-Lung01 & DESTINY-CRC02
All outcomes were assessed by independent central review (ICR) based on RECIST v1.1. In DESTINY-PanTumor02, ORR was 51.4% (95% CI: 41.7, 61.0) and median DOR was 19.4 months (range 1.3, 27.9+). In DESTINY-Lung01, ORR was 52.9% (95% CI: 27.8, 77.0) and median DOR was 6.9 months (range 4.0, 11.7+). In DESTINY-CRC02, ORR was 46.9% (95% CI: 34.3, 59.8), and DOR was 5.5 months (range 1.3+, 9.7+)
The review was conducted under Project Orbis, and included the Australian TGA, Brazil's ANVISA, Health Canada, and Singapore’s HSA