Newsroom
European Commission has approved INAQOVI® (oral decitabine and cedazuridine) for the treatment of adults with newly diagnosed acute myeloid leukaemia
European Commission has approved INAQOVI® (oral decitabine and cedazuridine) for the treatment of adults with newly diagnosed acute myeloid leukaemia
European Commission has approved INAQOVI® (oral decitabine and cedazuridine) as monotherapy for the treatment of adult patients with newly diagnosed acute myeloid leukaemia (AML) who are ineligible for standard induction chemotherapy
Approval is based on the results from the Phase 3 ASCERTAIN clinical trial investigating the pharmacokinetic exposure equivalence of the novel oral fixed-dose combination versus intravenous (IV) decitabine in AML patients
ASCERTAIN met its primary endpoint, with the orally administered decitabine and cedazuridine FDC showing pharmacokinetic exposure equivalence to a standard 5-day regimen of IV decitabine using a two-cycle, cross-over study design. Safety findings for the fixed-dose combination of decitabine and cedazuridine were generally consistent with those anticipated for IV decitabine
TEVIMBRA Receives European Commission Approval for the Treatment of Advanced or Metastatic ESCC
TEVIMBRA Receives European Commission Approval for the Treatment of Advanced or Metastatic ESCC
ARATIONALE 302 is a global, randomized, open-label, Phase 3 study (NCT03430843) designed to investigate the efficacy and safety of TEVIMBRA when compared with investigator’s choice chemotherapy as a second-line treatment for patients with unresectable, locally advanced or metastatic ESCC
Statistically significant and clinically meaningful survival benefit for TEVIMBRA compared with chemotherapy (HR 0.70 [95% CI: 0.57 - 0.85]; one-sided P=0.0001; median overall survival 8.6 vs 6.3 months)
The safety profile for TEVIMBRA was consistent with previous trials. The marketing authorization application included safety data for 1,972 patients who received TEVIMBRA monotherapy across seven clinical trials
FDA grants accelerated approval to Pfizer's Elrexfio for r/r multiple myeloma
FDA grants accelerated approval to Pfizer's Elrexfio for r/r multiple myeloma
ORR (N=97) was 57.7%, with a median follow-up of 11.1 months among responders, the median DOR was not reached
DOR rate at 6 months was 90.4% and at 9 months was 82.3%
Product awarded BTD, Priority Review, ODD. Orbis review inc. TGA, ANVISA, Health Canada & Swissmedic
U.S. FDA Approves TALVEY™ (talquetamab-tgvs), a First-in-Class Bispecific Therapy for the Treatment of Patients with Heavily Pretreated Multiple Myeloma
U.S. FDA Approves TALVEY™ (talquetamab-tgvs), a First-in-Class Bispecific Therapy for the Treatment of Patients with Heavily Pretreated Multiple Myeloma
Bispecific antibody targeting GPRC5D receptor showed an overall response rate of more than 70 percent with durable responses, including in patients previously treated with a bispecific antibody or CAR-T cell therapy
Accelerated approval is based on data from the single-arm Phase I/II MonumenTAL-1 study (Phase I: NCT03399799 and Phase II: NCT04634552) involving over 300 patients
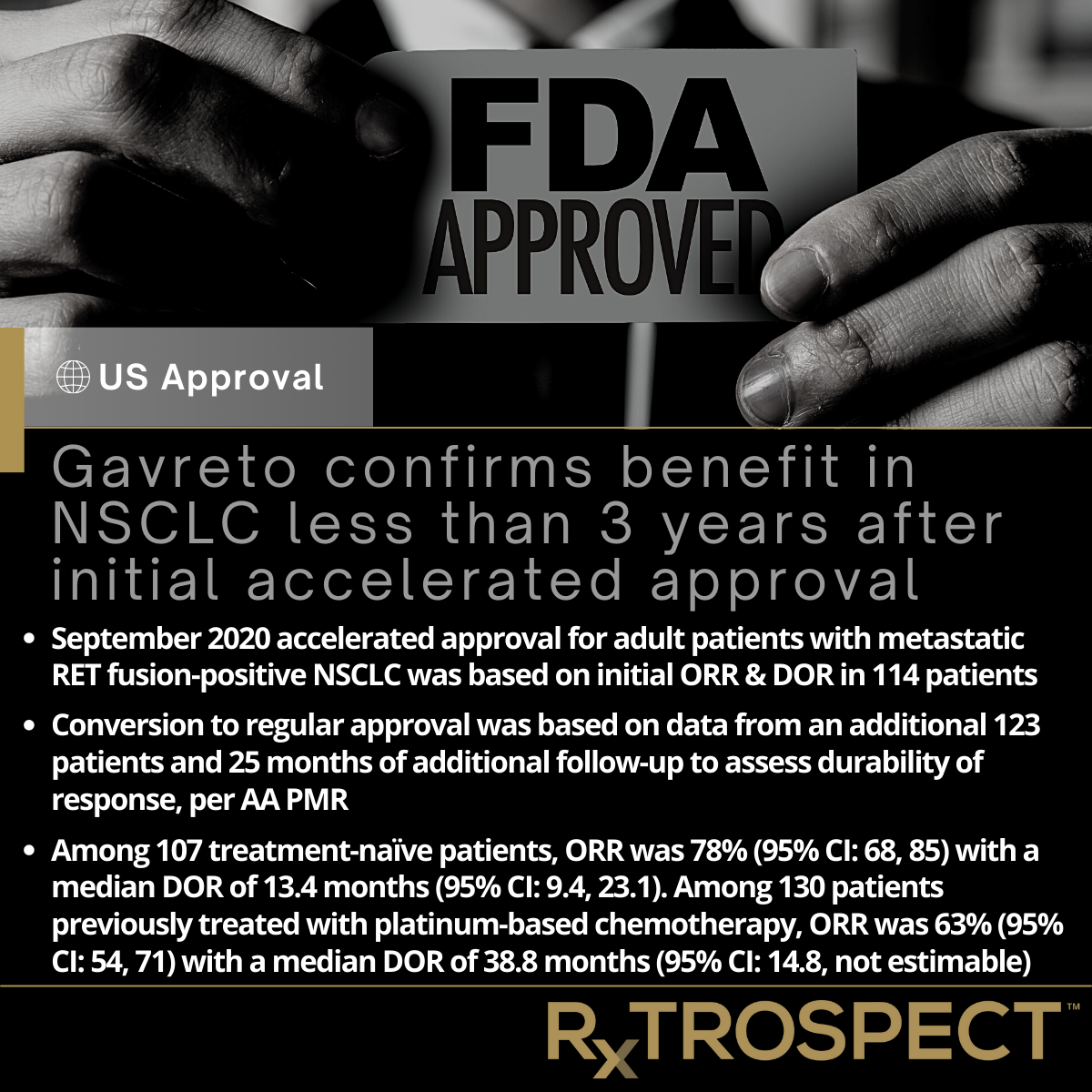
Gavreto confirms benefit in NSCLC less than 3 years after initial accelerated approval
Gavreto confirms benefit in NSCLC less than 3 years after initial accelerated approval
September 2020 accelerated approval for adult patients with metastatic RET fusion-positive NSCLC was based on initial ORR & DOR in 114 patients
Conversion to regular approval was based on data from an additional 123 patients and 25 months of additional follow-up to assess durability of response, per AA PMR
Among 107 treatment-naïve patients, ORR was 78% (95% CI: 68, 85) with a median DOR of 13.4 months (95% CI: 9.4, 23.1). Among 130 patients previously treated with platinum-based chemotherapy, ORR was 63% (95% CI: 54, 71) with a median DOR of 38.8 months (95% CI: 14.8, not estimable)
FDA Approves Daiichi Sankyo's NME quizartinib in frontline AML
FDA Approves Daiichi Sankyo's NME quizartinib in frontline AML
Efficacy of quizartinib with chemotherapy was evaluated in a Phase 3 randomized, double-blind, placebo-controlled trial of 539 patients with newly diagnosed FLT3-ITD positive AML
Patients were randomized (1:1) to receive quizartinib or PBO with induction and consolidation therapy and as maintenance monotherapy according to the initial assignment
Primary OS analysis after a minimum follow-up of 24 months showed a statistically significant improvement in OS for the quizartinib arm HR: 0.78; 95% CI: 0.62, 0.98; 2‑sided p=0.0324]
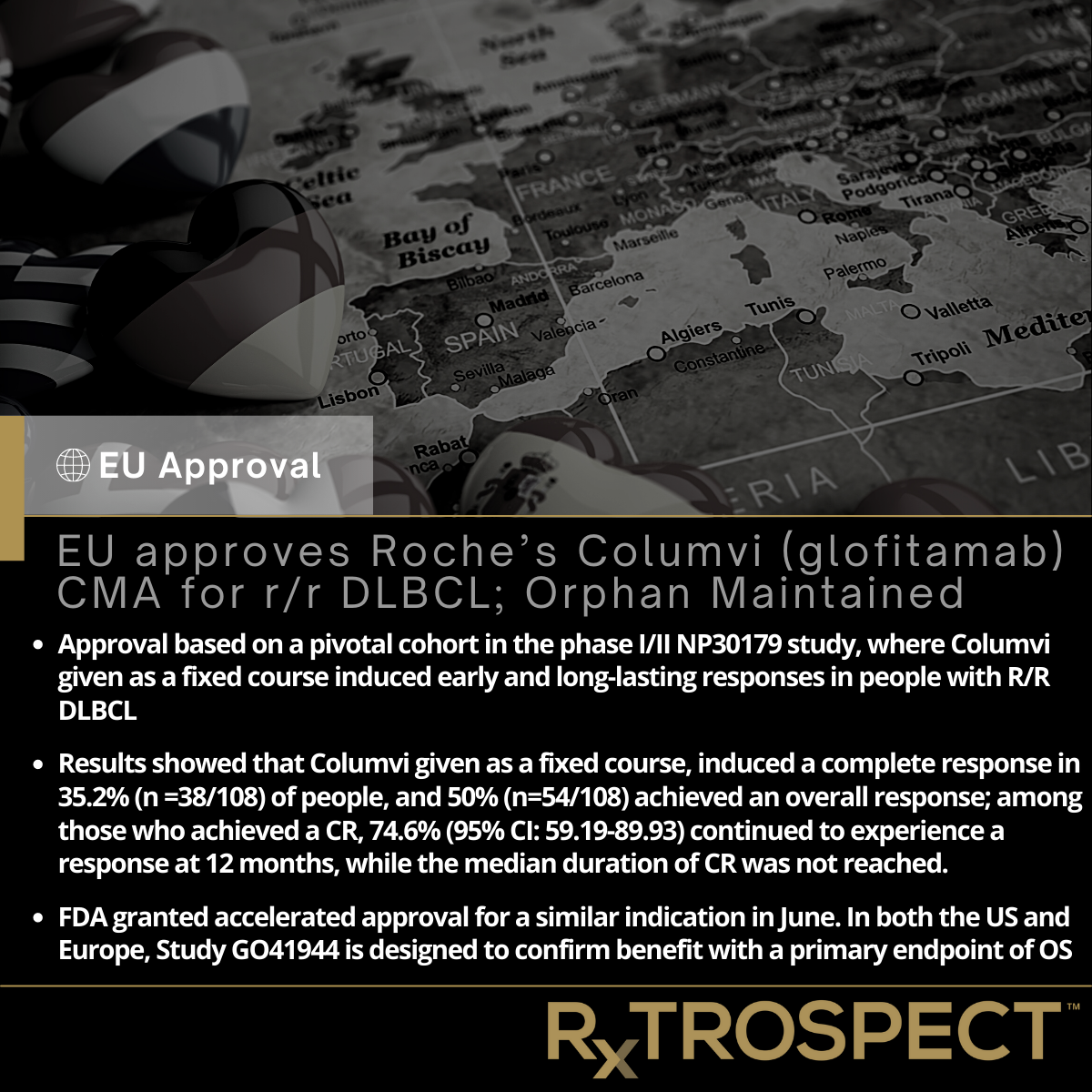
EU approves Roche’s Columvi (glofitamab) CMA for r/r DLBCL; Orphan Maintained
EU approves Roche’s Columvi (glofitamab) CMA for r/r DLBCL; Orphan Maintained
Approval based on a pivotal cohort in the phase I/II NP30179 study, where Columvi given as a fixed course induced early and long-lasting responses in people with R/R DLBCL
Results showed that Columvi given as a fixed course, induced a complete response in 35.2% (n =38/108) of people, and 50% (n=54/108) achieved an overall response; among those who achieved a CR, 74.6% (95% CI: 59.19-89.93) continued to experience a response at 12 months, while the median duration of CR was not reached.
FDA granted accelerated approval for a similar indication in June. In both the US and Europe, Study GO41944 is designed to confirm benefit with a primary endpoint of OS
FDA converts BLINCYTO (blinatumomab) to full approval for the treatment of adults and pediatric patients with MRD-positive ALL
FDA converts BLINCYTO (blinatumomab) to full approval for the treatment of adults and pediatric patients with MRD-positive ALL
Approval converts the 2018 accelerated approval, which was based on the single-arm BLAST trial (NCT 01207388) that included 86 patients
Follows completion of PMR 3366-2, to complete a randomized trial to verify clinical benefit of blinatumomab in pediatric patients in morphologic complete remission with detectable minimal residual disease
Amgen formally released from second PMR (3366-1) as the original accelerated approval provided two routes to confirm benefit (met by the fulfilment of PMR 3366-2)