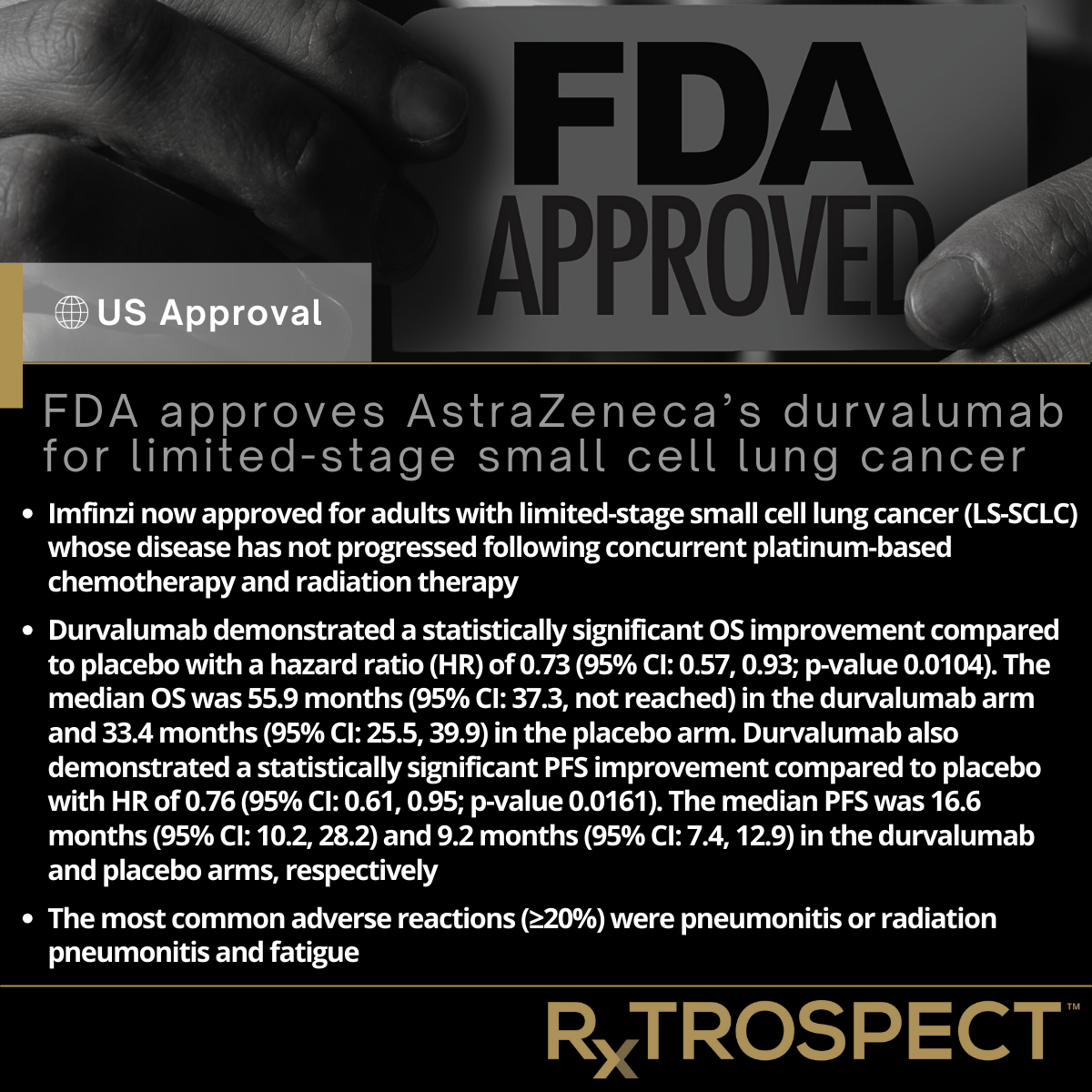
FDA approves AstraZeneca’s durvalumab for limited-stage small cell lung cancer
FDA approves AstraZeneca’s durvalumab for limited-stage small cell lung cancer
Imfinzi now approved for adults with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy
Durvalumab demonstrated a statistically significant OS improvement compared to placebo with a hazard ratio (HR) of 0.73 (95% CI: 0.57, 0.93; p-value 0.0104). The median OS was 55.9 months (95% CI: 37.3, not reached) in the durvalumab arm and 33.4 months (95% CI: 25.5, 39.9) in the placebo arm. Durvalumab also demonstrated a statistically significant PFS improvement compared to placebo with HR of 0.76 (95% CI: 0.61, 0.95; p-value 0.0161). The median PFS was 16.6 months (95% CI: 10.2, 28.2) and 9.2 months (95% CI: 7.4, 12.9) in the durvalumab and placebo arms, respectively
The most common adverse reactions (≥20%) were pneumonitis or radiation pneumonitis and fatigue
On December 4, 2024, the Food and Drug Administration approved durvalumab (Imfinzi, AstraZeneca) for adults with limited-stage small cell lung cancer (LS-SCLC) whose disease has not progressed following concurrent platinum-based chemotherapy and radiation therapy.
Full prescribing information for Imfinzi will be posted on Drugs@FDA.
Efficacy and Safety
Efficacy was evaluated in ADRIATIC (NCT03703297), a randomized, double-blind, placebo-controlled trial in 730 patients with LS-SCLC whose disease had not progressed following concurrent platinum-based chemotherapy and radiation therapy. Patients were randomized 1:1:1 to receive durvalumab as a single agent, durvalumab in combination with tremelimumab, or placebo.
The major efficacy outcome measures were overall survival (OS) and progression-free survival (PFS) assessed by blinded independent central review for the comparison between durvalumab as a single agent and placebo. Durvalumab demonstrated a statistically significant OS improvement compared to placebo with a hazard ratio (HR) of 0.73 (95% CI: 0.57, 0.93; p-value 0.0104). The median OS was 55.9 months (95% CI: 37.3, not reached) in the durvalumab arm and 33.4 months (95% CI: 25.5, 39.9) in the placebo arm. Durvalumab also demonstrated a statistically significant PFS improvement compared to placebo with HR of 0.76 (95% CI: 0.61, 0.95; p-value 0.0161). The median PFS was 16.6 months (95% CI: 10.2, 28.2) and 9.2 months (95% CI: 7.4, 12.9) in the durvalumab and placebo arms, respectively.
The most common adverse reactions (≥20%) were pneumonitis or radiation pneumonitis and fatigue.
The recommended durvalumab dose is 1,500 mg every 4 weeks for patients with a body weight of ≥30 kg and 20 mg/kg every 4 weeks for patients with a body weight of <30 kg until disease progression or unacceptable toxicity or a maximum of 24 months.
This review was conducted under Project Orbis, an initiative of the FDA Oncology Center of Excellence. Project Orbis provides a framework for concurrent submission and review of oncology drugs among international partners. For this review, FDA collaborated with the Australian Therapeutic Goods Administration (TGA), the Brazilian Health Regulatory Agency (ANVISA), Health Canada, and Switzerland’s Swissmedic (SMC). The European Medicines Agency (EMA) was an official observer of this review. The application reviews may be ongoing at the other regulatory agencies.
Expedited Programs
This review used the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment.
This application was granted priority review and breakthrough designation. FDA expedited programs are described in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
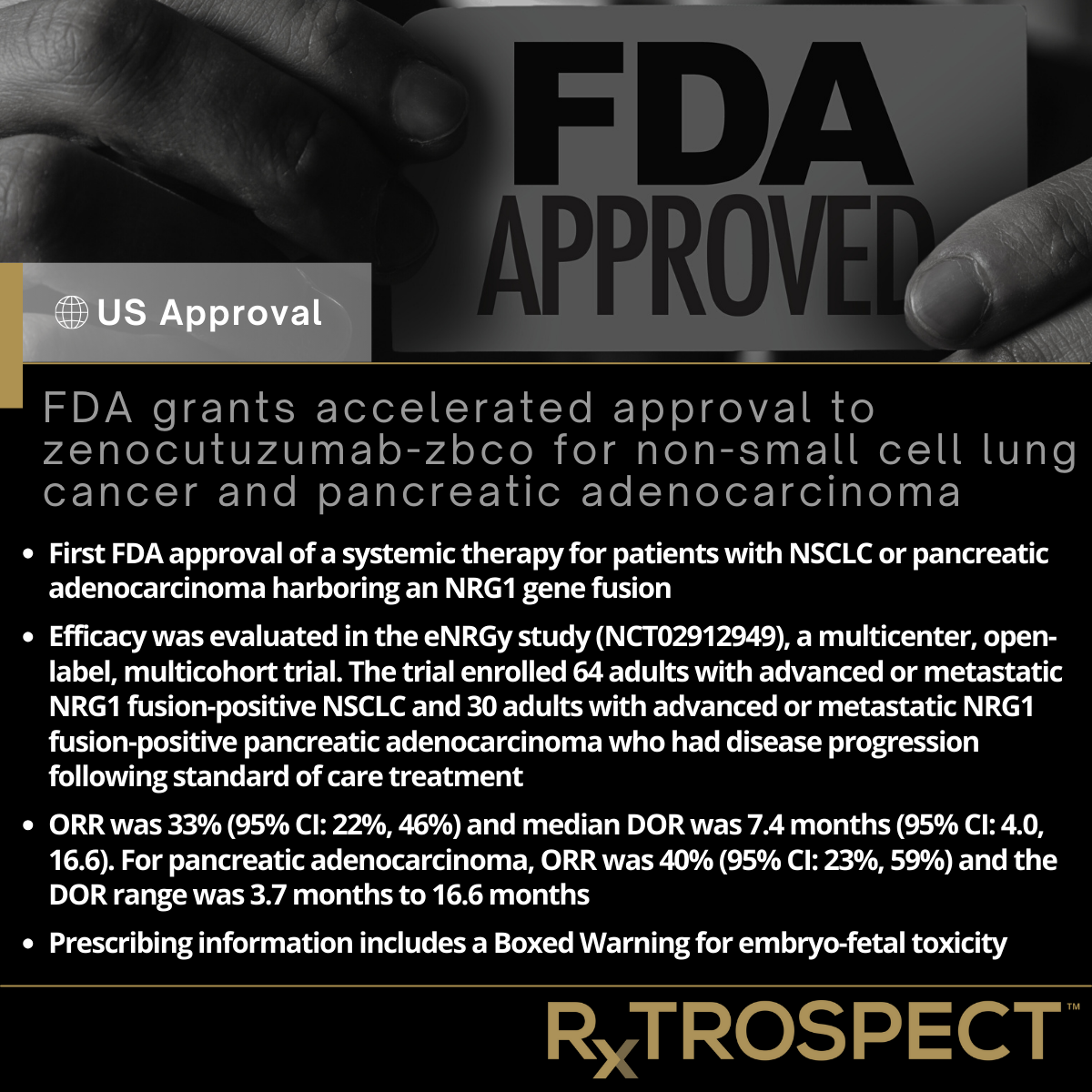
FDA grants accelerated approval to zenocutuzumab-zbco for non-small cell lung cancer and pancreatic adenocarcinoma
FDA grants accelerated approval to zenocutuzumab-zbco for non-small cell lung cancer and pancreatic adenocarcinoma
First FDA approval of a systemic therapy for patients with NSCLC or pancreatic adenocarcinoma harboring an NRG1 gene fusion.
Efficacy was evaluated in the eNRGy study (NCT02912949), a multicenter, open-label, multicohort trial. The trial enrolled 64 adults with advanced or metastatic NRG1 fusion-positive NSCLC and 30 adults with advanced or metastatic NRG1 fusion-positive pancreatic adenocarcinoma who had disease progression following standard of care treatment.
ORR was 33% (95% CI: 22%, 46%) and median DOR was 7.4 months (95% CI: 4.0, 16.6). For pancreatic adenocarcinoma, ORR was 40% (95% CI: 23%, 59%) and the DOR range was 3.7 months to 16.6 months.
Prescribing information includes a Boxed Warning for embryo-fetal toxicity
On December 4, 2024, the Food and Drug Administration granted accelerated approval to zenocutuzumab-zbco (Bizengri, Merus N.V.) for adults with the following:
advanced, unresectable, or metastatic non-small cell lung cancer (NSCLC) harboring a neuregulin 1 (NRG1) gene fusion with disease progression on or after prior systemic therapy, or
advanced, unresectable, or metastatic pancreatic adenocarcinoma harboring a NRG1 gene fusion with disease progression on or after prior systemic therapy.
This represents the first FDA approval of a systemic therapy for patients with NSCLC or pancreatic adenocarcinoma harboring an NRG1 gene fusion.
Full prescribing information for Bizengri will be posted on Drugs@FDA.
Efficacy was evaluated in the eNRGy study (NCT02912949), a multicenter, open-label, multicohort trial. The trial enrolled 64 adults with advanced or metastatic NRG1 fusion-positive NSCLC and 30 adults with advanced or metastatic NRG1 fusion-positive pancreatic adenocarcinoma who had disease progression following standard of care treatment. Identification of positive NRG1 gene fusion status was prospectively determined by next generation sequencing assays.
The major efficacy outcome measures were confirmed overall response rate (ORR) and duration of response (DOR), determined by blinded independent central review according to RECIST v1.1. For NSCLC, ORR was 33% (95% CI: 22%, 46%) and median DOR was 7.4 months (95% CI: 4.0, 16.6). For pancreatic adenocarcinoma, ORR was 40% (95% CI: 23%, 59%) and the DOR range was 3.7 months to 16.6 months.
In the pooled safety population, the most common adverse reactions (≥10%) were diarrhea, musculoskeletal pain, fatigue, nausea, infusion-related reactions, dyspnea, rash, constipation, vomiting, abdominal pain, and edema. The most common Grade 3 or 4 laboratory abnormalities (≥10%) were increased gamma-glutamyl transferase, decreased hemoglobin, decreased sodium, and decreased platelets. The prescribing information includes a Boxed Warning for embryo-fetal toxicity.
The recommended zenocutuzumab-zbco dose is 750 mg, as an intravenous infusion every 2 weeks, until disease progression or unacceptable toxicity.
Expedited Programs
This review used the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment.
This application was granted priority review, breakthrough designation, and orphan drug designation. FDA expedited programs are described in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
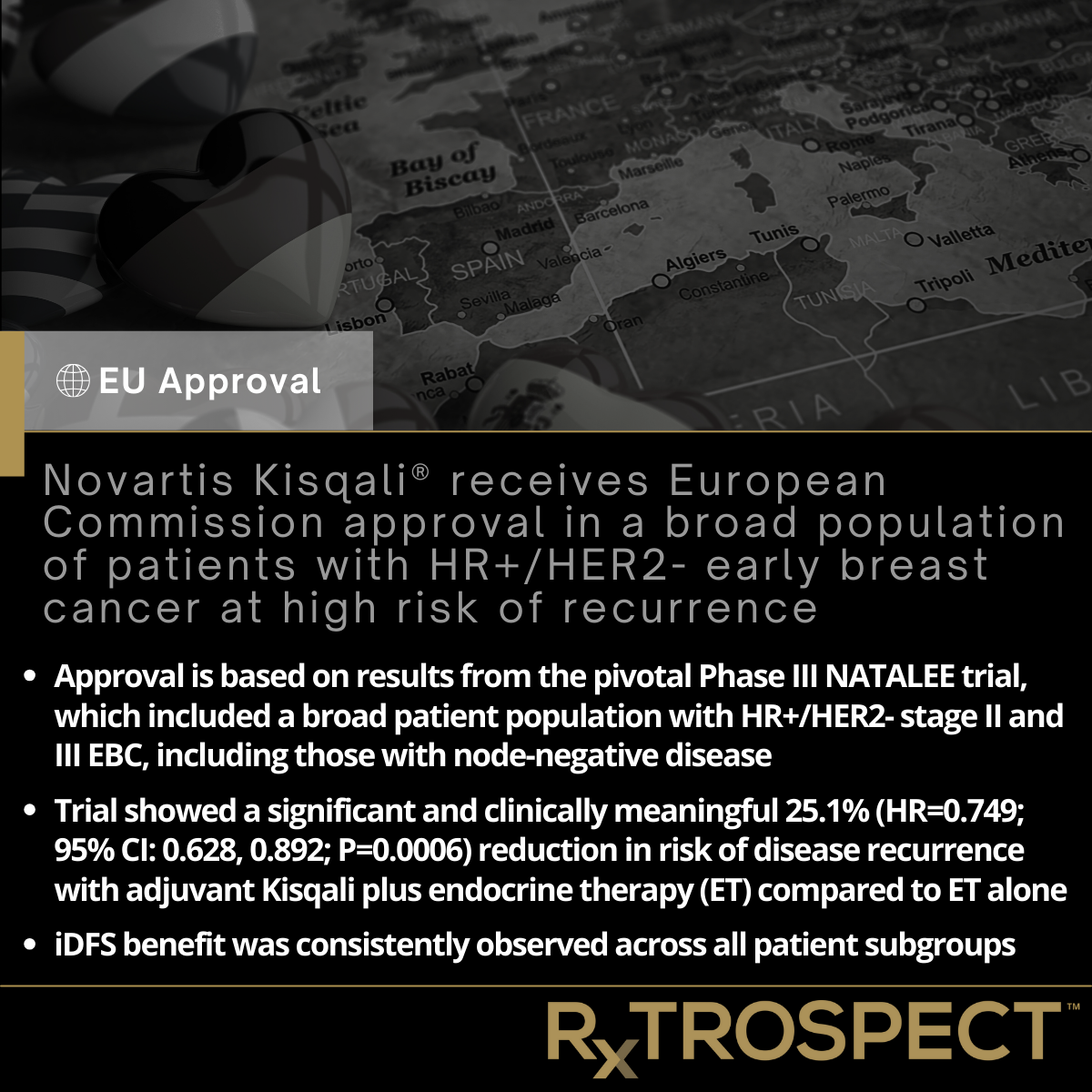
Novartis Kisqali® receives European Commission approval in a broad population of patients with HR+/HER2- early breast cancer at high risk of recurrence
Novartis Kisqali® receives European Commission approval in a broad population of patients with HR+/HER2- early breast cancer at high risk of recurrence
Approval is based on results from the pivotal Phase III NATALEE trial, which included a broad patient population with HR+/HER2- stage II and III EBC, including those with node-negative disease.
Trial showed a significant and clinically meaningful 25.1% (HR=0.749; 95% CI: 0.628, 0.892; P=0.0006) reduction in risk of disease recurrence with adjuvant Kisqali plus endocrine therapy (ET) compared to ET alone.
iDFS benefit was consistently observed across all patient subgroups.
Approval is based on Phase III NATALEE data showing Kisqali® (ribociclib) plus adjuvant endocrine therapy (ET) demonstrated clinically meaningful invasive disease-free survival (iDFS) benefit in patients with stage II or III HR+/HER2- early breast cancer (EBC), consistent across all subgroups1,2
With this broad indication, nearly twice as many EBC patients in Europe, including those with node-negative disease, could now be eligible for treatment with Kisqali to help reduce their risk of recurrence3
Despite ET, more than one-third of people diagnosed with stage II and III EBC will experience a return of their cancer in the long term, often as incurable advanced disease4,5
Recently presented four-year analysis of the ongoing NATALEE trial showed a deepening iDFS benefit after completion of three-year treatment period6
Basel, November 27, 2024 – Novartis announced today that the European Commission (EC) has approved Kisqali® (ribociclib) in combination with an aromatase inhibitor (AI) for the adjuvant treatment of patients with hormone receptor (HR)-positive, human epidermal growth factor receptor 2 (HER2)-negative early breast cancer (EBC) at high risk of recurrence1,7.
The approval is based on results from the pivotal Phase III NATALEE trial, which included a broad patient population with HR+/HER2- stage II and III EBC, including those with node-negative disease2. The trial showed a significant and clinically meaningful 25.1% (HR=0.749; 95% CI: 0.628, 0.892; P=0.0006) reduction in risk of disease recurrence with adjuvant Kisqali plus endocrine therapy (ET) compared to ET alone2. The invasive disease-free survival (iDFS) benefit was consistently observed across all patient subgroups2.
“For many patients diagnosed with stage II or III HR+/HER2- early breast cancer, the risk of their cancer coming back despite treatment with endocrine therapy remains high, even after decades,” said Michael Gnant, M.D., FACS, FEBS, Professor of Surgery at the Medical University of Vienna, Austria, and President of the Austrian Breast and Colorectal Study Group. “This approval represents a positive milestone for the early breast cancer community in Europe, including physicians who now have a new option to help reduce the risk of recurrence in a broader population of patients.”
In addition, Michael Untch, M.D., Professor and Head of the Clinic for Gynecology and Obstetrics, and Director of the Interdisciplinary Breast Cancer Center at Helios Klinikum Berlin-Buch, noted: “Adding a new treatment option to the HR+/HER2- early breast cancer armamentarium is encouraging news for both physicians and their patients – including patients with node-negative disease and additional risk factors. Ribociclib may now help many patients who are at risk of their cancer returning.”
Breast cancer is the most commonly diagnosed cancer in Europe8, with approximately 70% of cases diagnosed in the early stages of the disease9. Despite current treatment options, people with stage II and III HR+/HER2- EBC remain at risk of experiencing a return of their cancer in the long term, often as incurable advanced disease4,5.
"Breast cancer recurrence can be a lifelong concern for those living with the disease. Patients deserve access to treatment options that help minimize the risk of their cancer coming back and put their mind at ease,” said Iris Zemzoum, M.D., President, Europe, Novartis. “We are proud of this approval, which will help to address a key unmet need and improve health outcomes for a broader population of patients in Europe.”
This news follows the recent U.S. Food and Drug Administration (FDA) approval of Kisqali for EBC patients and recommendation as a Category 1 preferred breast cancer adjuvant treatment by the National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology (NCCN Guidelines®*)10,11. Kisqali has also achieved the highest score (A) on the European Society for Medical Oncology-Magnitude of Clinical Benefit Scale (ESMO-MCBS) for EBC12.
Regulatory review of Kisqali in EBC is ongoing worldwide. Following recent data announcements at ESMO 20246, Novartis will continue to evaluate NATALEE patients for longer-term outcomes, including overall survival.
*NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
About NATALEE
NATALEE is a global Phase III multi-center, randomized, open-label trial to evaluate the efficacy and safety of Kisqali® (ribociclib) with ET as an investigational adjuvant treatment versus ET alone in patients with stage II and III HR+/HER2- EBC, being conducted in collaboration with TRIO2,13. The adjuvant ET in both treatment arms was a non-steroidal aromatase inhibitor (NSAI; anastrozole or letrozole) and goserelin if applicable2,13. The primary endpoint of NATALEE is invasive disease-free survival (iDFS) as defined by the Standardized Definitions for Efficacy End Points (STEEP) criteria2,13. A total of 5,101 adult patients with HR+/HER2- EBC across 20 countries were randomized in the trial2,13.
About Kisqali® (ribociclib)
Kisqali® (ribociclib) is a selective cyclin-dependent kinase inhibitor, a class of drugs that help slow the progression of cancer by inhibiting two proteins called cyclin-dependent kinase 4 and 6 (CDK4/6). These proteins, when over-activated, can enable cancer cells to grow and divide too quickly. Targeting CDK4/6 with enhanced precision may play a role in ensuring that cancer cells do not continue to replicate uncontrollably.
Kisqali has been approved as a treatment for breast cancer by regulatory authorities in more than 100 countries worldwide, including the U.S. FDA and the European Commission8,14. In the U.S., Kisqali is indicated in combination with an AI as an adjuvant treatment of adults with HR+/HER2- stage II and III early breast cancer (EBC) at high risk of recurrence, as well as for the treatment of adults with HR+/HER2- advanced or metastatic breast cancer (MBC) as initial ET; Kisqali is also approved in the metastatic indication in combination with fulvestrant as initial ET or following disease progression on ET in post-menopausal women or in men14. In the EU, Kisqali is approved in combination with an AI for the adjuvant treatment of patients with HR+/HER2- EBC at high risk of recurrence. In pre- or perimenopausal women, or in men, the AI should be combined with a luteinising hormone-releasing hormone (LHRH) agonist; Kisqali is approved for the treatment of women with HR+/HER2- advanced or MBC in combination with either an AI or fulvestrant as initial ET or following disease progression. In pre- or peri-menopausal women, the ET should be combined with a LHRH8.
In EBC, it is the only CDK4/6 inhibitor recommended for both all node-positive disease as well as for patients with no nodal involvement with high-risk disease characteristics, such as tumor size >5 cm, or for tumors sized 2-5 cm, either Grade 2 with high genomic risk/Ki-67 ≥20% or Grade 38,14. Kisqali, in combination with an AI, has the highest score (A) on the ESMO-Magnitude of Clinical Benefit Scale for the adjuvant treatment of adults with stage II and III HR+/HER2- EBC, at high risk of recurrence12.
In MBC, Kisqali has consistently demonstrated statistically significant overall survival benefit across three Phase III trials15-25. The NCCN Guidelines® for breast cancer recommend ribociclib (Kisqali) as the only Category 1 preferred CDK4/6 inhibitor for first-line treatment of people living with HR+/HER2- when combined with an AI, making Kisqali the preferred first-line treatment of choice for U.S. prescribers in HR+/HER2- MBC26. In addition, Kisqali has the highest rating of any CDK4/6 inhibitor on the ESMO-Magnitude of Clinical Benefit Scale, achieving a score of five out of five for first-line pre-menopausal patients with HR+/HER2- advanced breast cancer27. Further, Kisqali in combination with either letrozole or fulvestrant has uniquely, among other CDK4/6 inhibitors, received a score of four out of five for post-menopausal patients with HR+/HER2- advanced breast cancer treated in the first line28.
Kisqali was developed by Novartis under a research collaboration with Astex Pharmaceuticals.
Please see full Prescribing Information for Kisqali, available at www.Kisqali.com.
About Novartis in Breast Cancer
For more than 30 years, Novartis has been at the forefront of driving scientific advancements for people touched by breast cancer and improving clinical practice in collaboration with the global community. With one of the most comprehensive breast cancer portfolios and pipeline, Novartis leads the industry in discovery of new therapies and combinations in HR+/HER2- breast cancer, the most common form of the disease.
Disclaimer
This press release contains forward-looking statements within the meaning of the United States Private Securities Litigation Reform Act of 1995. Forward-looking statements can generally be identified by words such as “potential,” “can,” “will,” “plan,” “may,” “could,” “would,” “expect,” “anticipate,” “look forward,” “believe,” “committed,” “investigational,” “pipeline,” “launch,” or similar terms, or by express or implied discussions regarding potential marketing approvals, new indications or labeling for the investigational or approved products described in this press release, or regarding potential future revenues from such products. You should not place undue reliance on these statements. Such forward-looking statements are based on our current beliefs and expectations regarding future events, and are subject to significant known and unknown risks and uncertainties. Should one or more of these risks or uncertainties materialize, or should underlying assumptions prove incorrect, actual results may vary materially from those set forth in the forward-looking statements. There can be no guarantee that the investigational or approved products described in this press release will be submitted or approved for sale or for any additional indications or labeling in any market, or at any particular time. Nor can there be any guarantee that such products will be commercially successful in the future. In particular, our expectations regarding such products could be affected by, among other things, the uncertainties inherent in research and development, including clinical trial results and additional analysis of existing clinical data; regulatory actions or delays or government regulation generally; global trends toward health care cost containment, including government, payor and general public pricing and reimbursement pressures and requirements for increased pricing transparency; our ability to obtain or maintain proprietary intellectual property protection; the particular prescribing preferences of physicians and patients; general political, economic and business conditions, including the effects of and efforts to mitigate pandemic diseases; safety, quality, data integrity or manufacturing issues; potential or actual data security and data privacy breaches, or disruptions of our information technology systems, and other risks and factors referred to in Novartis AG’s current Form 20-F on file with the US Securities and Exchange Commission. Novartis is providing the information in this press release as of this date and does not undertake any obligation to update any forward-looking statements contained in this press release as a result of new information, future events or otherwise.
About Novartis
Novartis is an innovative medicines company. Every day, we work to reimagine medicine to improve and extend people’s lives so that patients, healthcare professionals and societies are empowered in the face of serious disease. Our medicines reach more than 250 million people worldwide.
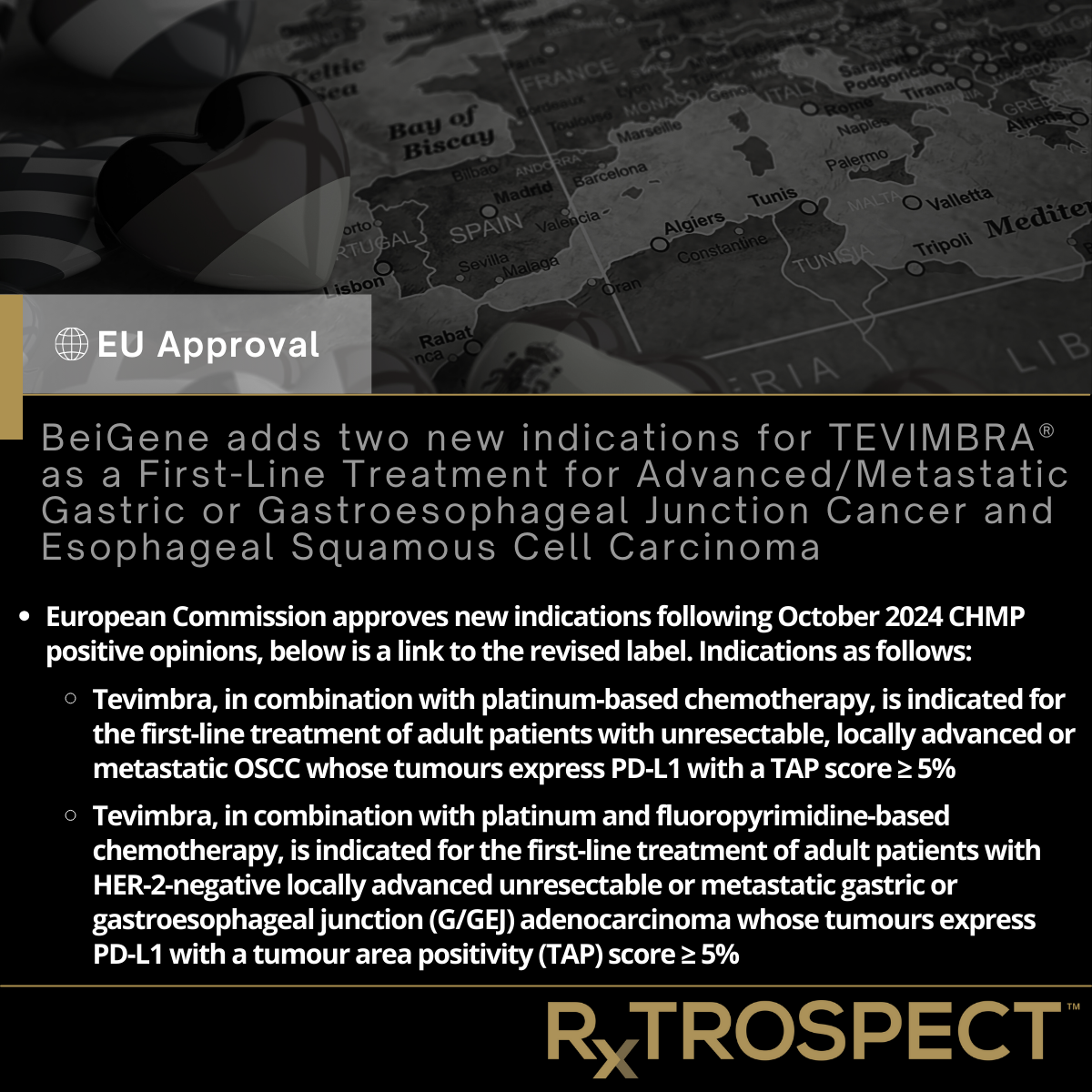
BeiGene adds two new indications for TEVIMBRA® as a First-Line Treatment for Advanced/Metastatic Gastric or Gastroesophageal Junction Cancer and Esophageal Squamous Cell Carcinoma
BeiGene adds two new indications for TEVIMBRA® as a First-Line Treatment for Advanced/Metastatic Gastric or Gastroesophageal Junction Cancer and Esophageal Squamous Cell Carcinoma
European Commission approves new indications following October 2024 CHMP positive opinions, below is a link to the revised label. Indications as follows:
Tevimbra, in combination with platinum-based chemotherapy, is indicated for the first-line treatment of adult patients with unresectable, locally advanced or metastatic OSCC whose tumours express PD-L1 with a TAP score ≥ 5%
Tevimbra, in combination with platinum and fluoropyrimidine-based chemotherapy, is indicated for the first-line treatment of adult patients with HER-2-negative locally advanced unresectable or metastatic gastric or gastroesophageal junction (G/GEJ) adenocarcinoma whose tumours express PD-L1 with a tumour area positivity (TAP) score ≥ 5%




























































FDA accelerated approval for zanidatamab in previously treated, unresectable or metastatic HER2-positive (IHC 3+) Biliary Tract Cancer
FDA accelerated approval for zanidatamab in previously treated, unresectable or metastatic HER2-positive (IHC 3+) Biliary Tract Cancer
Jazz Pharmaceuticals announced FDA accelerated approval of Ziihera® (zanidatamab-hrii) 50mg/mL for injection for intravenous use for the treatment of adults with previously treated, unresectable or metastatic HER2-positive (IHC 3+) biliary tract cancer (BTC), as detected by an FDA-approved test.
Ziihera was approved under accelerated approval based on a 52% objective response rate (ORR) and a median duration of response (DOR) of 14.9 months as determined by independent central review (ICR). The safety profile for Ziihera has been demonstrated in 80 patients in the HERIZON-BTC-01 trial.
The confirmatory, global, randomized Phase 3 trial HERIZON-BTC-302 (NCT06282575) is ongoing and is evaluating zanidatamab in combination with standard-of-care therapy versus standard-of-care therapy alone in the first-line setting for patients with HER2-positive BTC.
Ziihera is the first and only dual HER2-targeted bispecific antibody approved for HER2+ BTC in the U.S.
Ziihera received accelerated approval based on results including a 52% objective response rate and median duration of response of 14.9 months as determined by independent central review (ICR) from the HERIZON-BTC-01 clinical trial
Company to host investor webcast on Dec. 11, 2024
For U.S. media and investors only
DUBLIN, Nov. 20, 2024 /PRNewswire/ -- Jazz Pharmaceuticals plc (Nasdaq: JAZZ) today announced the U.S. Food and Drug Administration (FDA) accelerated approval of Ziihera® (zanidatamab-hrii) 50mg/mL for injection for intravenous use for the treatment of adults with previously treated, unresectable or metastatic HER2-positive (IHC 3+) biliary tract cancer (BTC), as detected by an FDA-approved test.1 Ziihera was approved under accelerated approval based on a 52% objective response rate (ORR) and a median duration of response (DOR) of 14.9 months as determined by independent central review (ICR). Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial.1 The Phase 3 HERIZON-BTC-302 confirmatory trial is ongoing to evaluate zanidatamab in combination with standard-of-care therapy versus standard-of-care therapy alone in the first-line setting for patients with HER2-positive BTC.
"BTC is a devastating disease with a poor prognosis and five-year survival rates under five percent in the metastatic setting. Patients with unresectable or metastatic HER2-positive BTC have had a high unmet need with limited treatment options and few approved therapies," said Rob Iannone, M.D., M.S.C.E., executive vice president, global head of research and development, and chief medical officer of Jazz Pharmaceuticals. "The approval of Ziihera, which previously received Breakthrough Therapy Designation from the FDA for this indication, is an important advance and offers the first and only dual HER2-targeted bispecific antibody and chemotherapy-free treatment for patients living with BTC. We look forward to advancing research of zanidatamab in BTC and other HER2-expressing solid tumors, with the goal of improving outcomes for more people diagnosed with these difficult-to-treat HER2-positive cancers."
The FDA approval of Ziihera is based on compelling data from the HERIZON-BTC-01 trial, which included the evaluation of zanidatamab as a single agent in previously treated HER2-positive (as determined by Roche Diagnostic's PATHWAY® anti-HER-2/neu (4B5) Rabbit Monoclonal Primary Antibody companion diagnostic) BTC and is the largest Phase 2b clinical trial to date specifically for this patient population. The trial achieved its primary endpoint of confirmed objective response rate (cORR) by independent central review (ICR) and results were presented at the American Society of Clinical Oncology (ASCO) Annual Meeting 2023, published in The Lancet Oncology, and included in the 2023 Best of ASCO® program. Longer follow-up data showing improvement upon previously reported DOR were reported at the ASCO Annual Meeting 2024.1
"As a clinical investigator and medical oncologist focused on advancing the care of patients with biliary tract and liver cancers, I have experienced firsthand the significant unmet need for effective therapies for patients with these diseases," said Dr. James Harding, associate attending, Gastrointestinal Oncology and Early Drug Development Services, at Memorial Sloan Kettering Cancer Center. "Zanidatamab has demonstrated antitumor activity and is now a new option for patients with HER2-positive biliary tract cancer. I look forward to continued and successful drug development for patients with biliary tract cancer."
"Metastatic biliary tract cancer, BTC, places a significant burden on patients, affecting their quality of life and their emotional and mental well-being, as well as that of their families," said Stacie Lindsey, CEO and founder of the Cholangiocarcinoma Foundation. "The approval of Ziihera offers a promising treatment option. It provides patients and their loved ones the possibility of more time together and an improved quality of life, which is invaluable for the entire BTC community."
The efficacy of Ziihera was evaluated in 62 patients with HER2-positive (IHC 3+ by central assessment) BTC in Cohort 1 of HERIZON-BTC-01, with major efficacy outcome measures of ORR and DOR as determined by ICR according to RECIST (Response Evaluation Criteria in Solid Tumors) v1.1.1 The study demonstrated an ORR of 52% [95% confidence interval (CI): 39, 65)] with a Kaplan Meier (KM) estimated median DOR of 14.9 months [95% CI: 7.4-not estimable] by ICR.1
Boxed Warning for Embryo-fetal toxicity: Exposure to Ziihera during pregnancy can cause embryo-fetal harm. Advise patients of the risk and need for effective contraception.1
The safety profile for Ziihera has been demonstrated in 80 patients in the HERIZON-BTC-01 trial. Serious adverse reactions occurred in 53% of patients who received Ziihera. The most common adverse reactions in patients who received Ziihera (≥ 20%) were diarrhea, infusion-related reaction, abdominal pain, and fatigue. Serious adverse reactions in > 2% of patients included biliary obstruction (15%), biliary tract infection (8%), sepsis (8%), pneumonia (5%), diarrhea (3.8%), gastric obstruction (3.8%), and fatigue (2.5%). A fatal adverse reaction of hepatic failure occurred in one patient who received Ziihera. Permanent discontinuation due to an adverse reaction occurred in 2.5% of patients who received Ziihera.1 See additional safety information below and full prescribing information https://pp.jazzpharma.com/pi/ziihera.en.USPI.pdf.
The confirmatory, global, randomized Phase 3 trial HERIZON-BTC-302 (NCT06282575) is ongoing and is evaluating zanidatamab in combination with standard-of-care therapy versus standard-of-care therapy alone in the first-line setting for patients with HER2-positive BTC. Continued approval for Ziihera may be contingent upon verification and description of clinical benefit in this confirmatory trial.
Zanidatamab is also being investigated in a number of additional tumor types, including Phase 3 trials in gastroesophageal adenocarcinomas (GEAs) and metastatic breast cancer (mBC). The HERIZON-GEA-01 trial evaluating the potential of zanidatamab plus chemotherapy with or without tislelizumab as first-line treatment for patients with advanced/metastatic HER2-positive GEAs. The EmpowHER-303 trial is evaluating the potential of zanidatamab in combination with physician's choice chemotherapy for the treatment of HER2-positive mBC for patients who have progressed on, or are intolerant to, previous trastuzumab deruxtecan treatment.
About the Phase 2b HERIZON-BTC-01 Trial
The Phase 2b HERIZON-BTC-01 trial of zanidatamab was an open-label, global Phase 2b study, which enrolled 87 patients with HER2-amplified, locally advanced unresectable or metastatic BTC (gallbladder cancer, intra-/extra-hepatic cholangiocarcinoma) into 2 cohorts and included 62 patients with HER2 IHC 3+ BTC. The trial evaluated zanidatamab (20 mg/kg IV every 2 weeks) in patients who had received prior gemcitabine-containing therapy. Patients with prior HER2-targeted therapy use were excluded from the trial. All patients were required to have HER2 status confirmed with tissue samples by a central lab. Patients (n=87) were assigned into two cohorts based on tumor IHC status: Cohort 1 (n=80) included patients who were IHC 2+/3+ (HER2-amplified) and Cohort 2 (n=7) included patients who were IHC 0/1+. Tumors were assessed every 8 weeks per RECIST v1.1. The primary endpoint was ORR by independent central review (ICR) in Cohort 1, with secondary endpoints including other efficacy and safety outcomes.
Investor Webcast on Wednesday, December 11, 2024
The company will host a webcast on Wednesday, December 11, 2024, at 4:30 p.m. ET / 9:30 p.m. GMT to provide investors an overview of clinical data, patient need and commercialization strategy for Ziihera. The webcast will include commentary from a leading BTC expert and the company's senior management.
Audio webcast/conference call:
U.S. Dial-In Number: +1 800 715 9871
Ireland Dial-In Number: +353 1800 943 926
Additional global dial-in numbers are available here.
Passcode: 4898380
A live webcast of the presentation may be accessed from the Investors section of the Jazz Pharmaceuticals website at www.jazzpharmaceuticals.com. Please connect to the website prior to the start of the presentation to ensure adequate time for any software downloads that may be necessary to listen to the webcast. An archive of the webcast will be available for at least one week following the presentation on the Investors section of the company's website at www.jazzpharmaceuticals.com.
More information about Ziihera, the Full Prescribing Information, including Boxed Warning and Patient Information, is available here.
About Ziihera® (zanidatamab-hrii)
Ziihera (zanidatamab-hrii) is a bispecific HER2-directed antibody that binds to two extracellular sites on HER2. Binding of zanidatamab-hrii with HER2 results in internalization leading to a reduction of the receptor on the tumor cell surface. Zanidatamab-hrii induces complement-dependent cytotoxicity (CDC), antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP). These mechanisms result in tumor growth inhibition and cell death in vitro and in vivo.1 In the United States, Ziihera is indicated for the treatment of adults with previously treated, unresectable or metastatic HER2-positive (IHC 3+) biliary tract cancer (BTC), as detected by an FDA-approved test.1 The U.S. Food and Drug Administration (FDA) granted accelerated approval for this indication based on overall response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial(s).1
Zanidatamab is not approved anywhere else in the world.
Zanidatamab is being developed in multiple clinical trials as a targeted treatment option for patients with solid tumors that express HER2. Zanidatamab is being developed by Jazz and BeiGene, Ltd. (BeiGene) under license agreements from Zymeworks, which first developed the molecule.
The FDA granted Breakthrough Therapy designation for zanidatamab development in patients with previously treated HER2 gene-amplified BTC, and two Fast Track designations for zanidatamab: one as a single agent for refractory BTC and one in combination with standard-of-care chemotherapy for 1L gastroesophageal adenocarcinoma (GEA). Additionally, zanidatamab has received Orphan Drug designations from FDA for the treatment of BTC and GEA, as well as Orphan Drug designation from the European Medicines Agency for the treatment of BTC and gastric cancer.
Important Safety Information
WARNING: EMBRYO-FETAL TOXICITY
Exposure to ZIIHERA during pregnancy can cause embryo-fetal harm. Advise patients
of the risk and need for effective contraception.
WARNINGS AND PRECAUTIONS
Embryo-Fetal Toxicity
ZIIHERA can cause fetal harm when administered to a pregnant woman. In literature reports, use of a HER2-directed antibody during pregnancy resulted in cases of oligohydramnios and oligohydramnios sequence manifesting as pulmonary hypoplasia, skeletal abnormalities, and neonatal death.
Verify the pregnancy status of females of reproductive potential prior to the initiation of ZIIHERA. Advise pregnant women and females of reproductive potential that exposure to ZIIHERA during pregnancy or within 4 months prior to conception can result in fetal harm. Advise females of reproductive potential to use effective contraception during treatment with ZIIHERA and for 4 months following the last dose of ZIIHERA.
Left Ventricular Dysfunction
ZIIHERA can cause decreases in left ventricular ejection fraction (LVEF). LVEF declined by >10% and decreased to <50% in 4.3% of 233 patients. Left ventricular dysfunction (LVD) leading to permanent discontinuation of ZIIHERA was reported in 0.9% of patients. The median time to first occurrence of LVD was 5.6 months (range: 1.6 to 18.7). LVD resolved in 70% of patients.
Assess LVEF prior to initiation of ZIIHERA and at regular intervals during treatment. Withhold dose or permanently discontinue ZIIHERA based on severity of adverse reactions.
The safety of ZIIHERA has not been established in patients with a baseline ejection fraction that is below 50%.
Infusion-Related Reactions
ZIIHERA can cause infusion-related reactions (IRRs). An IRR was reported in 31% of 233 patients treated with ZIIHERA as a single agent in clinical studies, including Grade 3 (0.4%), and Grade 2 (25%). IRRs leading to permanent discontinuation of ZIIHERA were reported in 0.4% of patients. IRRs occurred on the first day of dosing in 28% of patients; 97% of IRRs resolved within one day.
Prior to each dose of ZIIHERA, administer premedications to prevent potential IRRs. Monitor patients for signs and symptoms of IRR during ZIIHERA administration and as clinically indicated after completion of infusion. Have medications and emergency equipment to treat IRRs available for immediate use.
If an IRR occurs, slow, or stop the infusion, and administer appropriate medical management. Monitor patients until complete resolution of signs and symptoms before resuming. Permanently discontinue ZIIHERA in patients with recurrent severe or life-threatening IRRs.
Diarrhea
ZIIHERA can cause severe diarrhea.
Diarrhea was reported in 48% of 233 patients treated in clinical studies, including Grade 3 (6%) and Grade 2 (17%). If diarrhea occurs, administer antidiarrheal treatment as clinically indicated. Perform diagnostic tests as clinically indicated to exclude other causes of diarrhea. Withhold or permanently discontinue ZIIHERA based on severity.
ADVERSE REACTIONS
Serious adverse reactions occurred in 53% of 80 patients with unresectable or metastatic HER2-positive BTC who received ZIIHERA. Serious adverse reactions in >2% of patients included biliary obstruction (15%), biliary tract infection (8%), sepsis (8%), pneumonia (5%), diarrhea (3.8%), gastric obstruction (3.8%), and fatigue (2.5%). A fatal adverse reaction of hepatic failure occurred in one patient who received ZIIHERA.
The most common adverse reactions in 80 patients with unresectable or metastatic HER2-positive BTC who received ZIIHERA (≥20%) were diarrhea (50%), infusion-related reaction (35%), abdominal pain (29%), and fatigue (24%).
USE IN SPECIFIC POPULATIONS
Pediatric Use
Safety and efficacy of ZIIHERA have not been established in pediatric patients.
Geriatric Use
Of the 80 patients who received ZIIHERA for unresectable or metastatic HER2-positive BTC, there were 39 (49%) patients 65 years of age and older. Thirty-seven (46%) were aged 65-74 years old and 2 (3%) were aged 75 years or older.
No overall differences in safety or efficacy were observed between these patients and younger adult patients.
About Biliary Tract Cancer
BTC, including gallbladder cancer and intrahepatic and extrahepatic cholangiocarcinoma, account for <1% of all adult cancers globally and are often associated with a poor prognosis.2,3 The human epidermal growth factor receptor 2 (HER2) is a well-validated target for antitumor therapy in other cancers. Across the U.S., Europe, and Japan, approximately 12,000 people are diagnosed with HER2+ BTC annually.4,5,6,7
About Jazz Pharmaceuticals
Jazz Pharmaceuticals plc (Nasdaq: JAZZ) is a global biopharma company whose purpose is to innovate to transform the lives of patients and their families. We are dedicated to developing life-changing medicines for people with serious diseases—often with limited or no therapeutic options. We have a diverse portfolio of marketed medicines, including leading therapies for sleep disorders and epilepsy, and a growing portfolio of cancer treatments. Our patient-focused and science-driven approach powers pioneering research and development advancements across our robust pipeline of innovative therapeutics in oncology and neuroscience. Jazz is headquartered in Dublin, Ireland with research and development laboratories, manufacturing facilities and employees in multiple countries committed to serving patients worldwide. Please visit www.jazzpharmaceuticals.com for more information.
AbbVie Receives European Approval of ELAHERE® (mirvetuximab soravtansine) for the Treatment of Platinum-Resistant Ovarian Cancer
AbbVie Receives European Approval of ELAHERE® (mirvetuximab soravtansine) for the Treatment of Platinum-Resistant Ovarian Cancer
ELAHERE is the first and only folate receptor alpha (FRɑ)-directed ADC approved in the Europe; supported by data from MIRASOL: a global, Phase 3 open-label, randomized, controlled trial.
Results presented at the 2023 ASCO demonstrated a 35% reduction in the risk of tumor progression or death in patients treated in the ELAHERE arm compared with the investigator's choice (IC) chemotherapy arm, which represented an improvement in PFS [HR 0.65 (95% CI: 0.52, 0.81; p<0.0001)].
ELAHERE also demonstrated improvement in OS compared with IC chemotherapy, representing a 33% reduction in the risk of death in the ELAHERE arm in comparison to the IC chemotherapy arm [HR 0.67 (95% CI: 0.50, 0.89; p=0.0046)].
The most common adverse reactions with ELAHERE were blurred vision, nausea, diarrhea, fatigue, abdominal pain, keratopathy, dry eye, constipation, vomiting, decreased appetite, peripheral neuropathy, headache, asthenia, increased aspartate aminotransferase and arthralgia. The most commonly reported serious adverse reaction was pneumonitis.
ELAHERE is the first and only novel therapy approved in the European Union specifically for patients with folate receptor-alpha (FRα) positive, platinum-resistant ovarian cancer
ELAHERE represents the first treatment to demonstrate an overall survival benefit in a Phase 3 trial in platinum-resistant ovarian cancer compared with chemotherapy
VENTANA FOLR1 (FOLR1-2.1) RxDx Assay, the companion diagnostic to identify ovarian cancer patients eligible for ELAHERE, also receives CE Mark
NORTH CHICAGO, Ill., Nov. 18, 2024 /PRNewswire/ -- AbbVie (NYSE: ABBV) today announced the European Commission (EC) granted marketing authorization for ELAHERE® (mirvetuximab soravtansine) for the treatment of adult patients with folate receptor-alpha (FRα) positive, platinum-resistant high grade serous epithelial ovarian, fallopian tube or primary peritoneal cancer who have received one to three prior systemic treatment regimens. ELAHERE is the first and only folate receptor alpha (FRɑ)-directed antibody drug conjugate (ADC) medicine approved in the European Union (EU), as well as Iceland, Liechtenstein, Norway, and Northern Ireland.
"It's been 10 years since a new treatment for platinum-resistant ovarian cancer was approved in the EU, and now oncologists have an effective, new, targeted treatment option for these patients," said Toon Van Gorp, Professor of Gynaecological Oncology at the University of Leuven.
Ovarian cancer is one of the leading causes of death from gynecological cancers worldwide.i Most patients present with late-stage disease and will typically undergo surgery followed by platinum-based chemotherapy. Unfortunately, most patients eventually develop platinum-resistant disease.ii Historically, treatment options for patients with platinum-resistant ovarian cancer (PROC) have been limited, and those available often result in adverse events which can negatively impact quality of life.iii
"Ovarian cancer can be devastating, taking women away from precious moments with their family, disrupting careers and the many other important contributions that women make to society," said Clara Mackay, CEO, World Ovarian Cancer Coalition. "In Europe, ovarian cancer is three times more deadly than breast cancer, and having new innovative options allows us to work toward a world where everyone living with ovarian cancer has the best chance of survival and the best quality of life possible, no matter where they live."
In approximately one third of people living with ovarian cancer, the folate-receptor alpha (FRα) biomarker is highly expressediv (≥75% of tumor cells with ≥2+ membrane staining intensity). To determine biomarker status, patients can be tested with Roche's VENTANA® FOLR1 (FOLR1-2.1) RxDx Assay at diagnosis or at the first sign of resistance to platinum-based chemotherapy. AbbVie collaborated with Roche Diagnostics on the newly approved immunohistochemistry (IHC) companion diagnostic test to identify patients who may be eligible for ELAHERE.
"The approval of ELAHERE by the European Commission provides a much needed clinically meaningful option for patients who receive the heartbreaking news their ovarian cancer has returned, fearing what's next in their treatment journey after they've developed platinum-resistance," said Roopal Thakkar, M.D., executive vice president, research and development, chief scientific officer, AbbVie.
The marketing authorization of ELAHERE is supported by data from MIRASOL: a global, Phase 3 open-label, randomized, controlled trial.
Trial participants were 18 years of age or older with disease that had progressed while on or after one to three lines of previous therapy. Patient tumors had to express high levels of FRɑ (≥75% of tumor cells with ≥2+ membrane intensity), assessed using the VENTANA FOLR1 (FOLR1-2.1) RxDx Assay. The primary endpoint was investigator-assessed progression-free survival (PFS). Key secondary endpoints included objective response rate (ORR) and overall survival (OS).
Results presented at the 2023 American Society of Clinical Oncology (ASCO) Annual Meeting demonstrated a 35% reduction in the risk of tumor progression or death in patients treated in the ELAHERE arm compared with the investigator's choice (IC) chemotherapy arm, which represented an improvement in PFS [HR 0.65 (95% CI: 0.52, 0.81; p<0.0001)].
ELAHERE also demonstrated improvement in OS compared with IC chemotherapy, representing a 33% reduction in the risk of death in the ELAHERE arm in comparison to the IC chemotherapy arm [HR 0.67 (95% CI: 0.50, 0.89; p=0.0046)].
The most common adverse reactions with ELAHERE were blurred vision, nausea, diarrhea, fatigue, abdominal pain, keratopathy, dry eye, constipation, vomiting, decreased appetite, peripheral neuropathy, headache, asthenia, increased aspartate aminotransferase and arthralgia. The most commonly reported serious adverse reaction was pneumonitis.
Data from the Phase 3 MIRASOL Trial were also published in the New England Journal of Medicine (NEJM).
About the Phase 3 MIRASOL Trial
MIRASOL is a global Phase 3 open-label, randomized, controlled trial that enrolled 453 patients to compare the efficacy and safety of mirvetuximab soravtansine with the investigator's choice of single-agent chemotherapy (weekly paclitaxel, pegylated liposomal doxorubicin, or topotecan) in the treatment of platinum-resistant, high-grade serous ovarian cancer whose tumors express high levels of FRα (≥75% of cells with ≥2+ staining intensity), confirmed with a validated test. Participants had previously received one to three lines of prior therapy. The primary endpoint was investigator-assessed progression-free survival (PFS). Key secondary endpoints included objective response rate (ORR) and overall survival (OS).
More information can be found on www.clinicaltrials.gov (NCT 04209855).
About ELAHERE (mirvetuximab soravtansine)
ELAHERE is a first-in-class ADC composed of a folate receptor alpha binding antibody, cleavable linker, and the maytansinoid payload DM4, a potent tubulin inhibitor designed to kill the targeted cancer cells.
Mirvetuximab soravtansine (approved under the brand name ELAHERE®) was granted approval by the European Commission in November 2024, and was granted full FDA approval in the United States in March 2024.
Marketing authorization submissions for mirvetuximab soravtansine are under review in multiple other countries.
EU Indication and Important Safety Information about Elahere® ▼ (mirvetuximab soravtansine)
Indication
ELAHERE (mirvetuximab soravtansine) as monotherapy is indicated for the treatment of adult patients with folate receptor-alpha (FRα) positive, platinum-resistant high grade serous epithelial ovarian, fallopian tube, or primary peritoneal cancer who have received one to three prior systemic treatment regimens.
FDA approves revumenib for relapsed or refractory acute leukemia with a KMT2A translocation
FDA approves revumenib for relapsed or refractory acute leukemia with a KMT2A translocation
Efficacy was evaluated in a single-arm cohort of an open-label, multicenter trial (NCT04065399) in 104 adult and pediatric patients (at least 30 days old) with R/R acute leukemia with a KMT2A translocation.
CR+CRh rate was 21.2% (95% CI: 13.8, 30.3), and the median CR+CRh duration was 6.4 months (95% CI: 2.7, not estimable).
Among the 83 patients dependent on RBC and/or platelet transfusions at baseline, 12 (14%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 21 patients independent of both RBC and platelet transfusions at baseline, 10 (48%) remained transfusion independent during any 56-day post-baseline period.
Due to an anticipated delay in commercial availability of the lowest dose strength of revumenib, which may be used to treat patients who weigh < 40 kg, revumenib will be available through an expanded access program to allow for dosing of patients who weigh < 40 kg (information available here: NCT05918913).
This review used RTOR pilot program, which streamlined data submission prior to the filing of the entire clinical application, and the Assessment Aid. FDA approved this application 6 weeks early.
On November 15, 2024, the Food and Drug Administration approved revumenib (Revuforj, Syndax Pharmaceuticals, Inc.), a menin inhibitor, for relapsed or refractory acute leukemia with a lysine methyltransferase 2A gene (KMT2A) translocation in adult and pediatric patients 1 year and older.
Full prescribing information for Revuforj will be posted on Drugs@FDA.
Efficacy and Safety
Efficacy was evaluated in a single-arm cohort of an open-label, multicenter trial (SNDX-5613-0700, NCT04065399; AUGMENT-101) in 104 adult and pediatric patients (at least 30 days old) with relapsed or refractory (R/R) acute leukemia with a KMT2A translocation. Patients with an 11q23 partial tandem duplication were excluded. Revumenib was administered until disease progression, unacceptable toxicity, failure to achieve morphological leukemia-free state by 4 cycles of treatment, or hematopoietic stem cell transplantation (HSCT).
The main efficacy outcome measures were complete remission (CR) plus CR with partial hematologic recovery (CRh), the duration of CR+CRh, and conversion from transfusion dependence to independence. The CR+CRh rate was 21.2% (95% CI: 13.8, 30.3), and the median CR+CRh duration was 6.4 months (95% CI: 2.7, not estimable). Of the 22 patients achieving CR or CRh, the median time to CR or CRh was 1.9 months (range: 0.9, 5.6 months). Among the 83 patients dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 12 (14%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 21 patients independent of both RBC and platelet transfusions at baseline, 10 (48%) remained transfusion independent during any 56-day post-baseline period.
The most common adverse reactions (≥20%) were hemorrhage, nausea, increased phosphate, musculoskeletal pain, infection, increased aspartate aminotransferase, febrile neutropenia, increased alanine aminotransferase, increased intact parathyroid hormone, bacterial infection, diarrhea, differentiation syndrome, electrocardiogram QT prolonged, decreased phosphate, increased triglycerides, decreased potassium, decreased appetite, constipation, edema, viral infection, fatigue, and increased alkaline phosphatase.
The recommended revumenib dose varies by patient weight and concomitant use of strong CYP3A4 inhibitors. See the prescribing information for specific dosage information. Due to an anticipated delay in commercial availability of the lowest dose strength of revumenib, which may be used to treat patients who weigh < 40 kg, revumenib will be available through an expanded access program to allow for dosing of patients who weigh < 40 kg (information available here: NCT05918913).
This review used the Real-Time Oncology Review (RTOR) pilot program, which streamlined data submission prior to the filing of the entire clinical application, and the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment. The FDA approved this application 6 weeks ahead of the FDA goal date.
Expedited Programs
This application was granted priority review. Revumenib has breakthrough designation and orphan drug designation. FDA expedited programs are described in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics.
FDA approves obecabtagene autoleucel for adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia
FDA approves obecabtagene autoleucel for adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia
Efficacy was evaluated in FELIX (NCT04404660), an open-label, multicenter, single-arm trial that enrolled adults with relapsed or refractory CD19-positive B-cell ALL.
Of the 65 patients evaluable for efficacy, 27 patients (42%; 95% CI: 29%, 54%) achieved CR within 3 months. Median duration of CR achieved within 3 months was 14.1 months (95% CI: 6.1, not reached). Label has a boxed warning for CRS, ICANS and T cell malignancies.
Product granted regenerative medicine advanced therapy designation and orphan drug designation. This is the first FDA approval for Autolus Therapeutics.
On November 8, 2024, the Food and Drug Administration approved obecabtagene autoleucel (Aucatzyl, Autolus Inc.), a CD19-directed genetically modified autologous T cell immunotherapy, for adults with relapsed or refractory B-cell precursor acute lymphoblastic leukemia (ALL).
Full prescribing information for Aucatzyl will be posted on Drugs@FDA.
Efficacy and Safety
Efficacy was evaluated in FELIX (NCT04404660), an open-label, multicenter, single-arm trial that enrolled adults with relapsed or refractory CD19-positive B-cell ALL. Enrolled patients were required to have relapsed following a remission lasting 12 months or less, relapsed or refractory ALL following two or more prior lines of systemic therapy, or disease that was relapsed or refractory 3 or more months after allogeneic stem cell transplantation.
The major efficacy outcome measures were rate and duration of complete remission (CR) achieved within 3 months after infusion. Additional outcome measures were rate and duration of overall complete remission which includes complete remission and complete remission with incomplete hematologic recovery (CRi), at any time. Of the 65 patients evaluable for efficacy, 27 patients (42%; 95% confidence interval [CI]: 29%, 54%) achieved CR within 3 months. The median duration of CR achieved within 3 months was 14.1 months (95% CI: 6.1, not reached).
The prescribing information has a boxed warning for cytokine release syndrome (CRS), immune effector cell-associated neurotoxicity syndrome (ICANS) and T cell malignancies. CRS occurred in 75% (Grade 3, 3%) and neurologic toxicities occurred in 64% (Grade ≥3, 12%), including ICANS in 24% (Grade ≥3, 7%).The most common non-laboratory adverse reactions (incidence ≥ 20%) included CRS, infections-pathogen unspecified, musculoskeletal pain, viral infections, fever, nausea, bacterial infectious disorders, diarrhea, febrile neutropenia, ICANS, hypotension, pain, fatigue, headache, encephalopathy, and hemorrhage.
The total recommended dose of obecabtagene autoleucel is 410 X 106 CD19 chimeric antigen receptor (CAR)-positive viable T cells to be administered as split dose infusion on Day 1 and Day 10 (±2 days) based on bone marrow blast assessment and preceded by fludarabine and cyclophosphamide lymphodepleting chemotherapy.
Expedited Programs
This review used the Assessment Aid, a voluntary submission from the applicant to facilitate the FDA’s assessment.
This application was granted regenerative medicine advanced therapy designation and orphan drug designation. FDA expedited programs are described in the Guidance for Industry: Expedited Programs for Serious Conditions-Drugs and Biologics. A description of FDA expedited programs for RMAT is in the Guidance for Industry: Expedited Programs for Regenerative Medicine Therapies for Serious Conditions.